Prevention Impacts Simulation Model (PRISM) Core Contributors - PowerPoint PPT Presentation
1 / 23
Title:
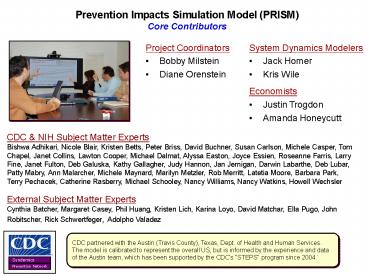
Prevention Impacts Simulation Model (PRISM) Core Contributors
Description:
Title: PowerPoint Presentation Author: Bobby Milstein Last modified by: Bobby Created Date: 10/2/2001 12:13:23 AM Document presentation format: On-screen Show – PowerPoint PPT presentation
Number of Views:184
Avg rating:3.0/5.0
Title: Prevention Impacts Simulation Model (PRISM) Core Contributors
1
Prevention Impacts Simulation Model (PRISM)Core
Contributors
- System Dynamics Modelers
- Jack Homer
- Kris Wile
- Project Coordinators
- Bobby Milstein
- Diane Orenstein
- Economists
- Justin Trogdon
- Amanda Honeycutt
CDC NIH Subject Matter ExpertsBishwa Adhikari,
Nicole Blair, Kristen Betts, Peter Briss, David
Buchner, Susan Carlson, Michele Casper, Tom
Chapel, Janet Collins, Lawton Cooper, Michael
Dalmat, Alyssa Easton, Joyce Essien, Roseanne
Farris, Larry Fine, Janet Fulton, Deb Galuska,
Kathy Gallagher, Judy Hannon, Jan Jernigan,
Darwin Labarthe, Deb Lubar, Patty Mabry, Ann
Malarcher, Michele Maynard, Marilyn Metzler, Rob
Merritt, Latetia Moore, Barbara Park, Terry
Pechacek, Catherine Rasberry, Michael Schooley,
Nancy Williams, Nancy Watkins, Howell Wechsler
External Subject Matter ExpertsCynthia Batcher,
Margaret Casey, Phil Huang, Kristen Lich, Karina
Loyo, David Matchar, Ella Pugo, John Robitscher,
Rick Schwertfeger, Adolpho Valadez
CDC partnered with the Austin (Travis County),
Texas, Dept. of Health and Human Services. The
model is calibrated to represent the overall US,
but is informed by the experience and data of the
Austin team, which has been supported by the
CDCs STEPS program since 2004.
2
Prevention Impacts Simulation Model (PRISM)
- Represents multiple interacting risks and
interventions for heart disease, stroke, and
related chronic diseases medical, behavioral,
social, environmental - Begun in 2007 (now version 2i) and it remains a
work-in-progress - Engaged subject matter experts from 12
organizations (N30), and 100s of policy
officials, including a deep collaboration with
local leaders in Austin, Texas - Integrates best available information in a single
testable model to support prospective planning
and evaluation - Explores the likely effects of local
interventions (i.e., changes in local
options/exposures/services that affect behavior
and/or health status) - To what extent might adverse events and costs be
reduced? - How can policymakers balance interventions for
best effect with limited resources?
References Homer J, Milstein B, Wile K,
Trogdon J, Huang P, Labarthe D, Orenstein D.
Simulating and evaluating local interventions to
improve cardiovascular health. Preventing
Chronic Disease, 2009 (in press). Homer J,
Milstein B, Wile K, Pratibhu P, Farris R,
Orenstein D. Modeling the local dynamics of
cardiovascular health risk factors, context, and
capacity. Preventing Chronic Disease 20085(2).
Available at lthttp//www.cdc.gov/pcd/issues/2008/
apr/07_0230.htm
3
The Popular (and Professional) View of Chronic
Disease Challenges is Largely One Headline after
Another
JunkFood
Tobacco
PhysicalActivity
Obesity
Heart Disease Stroke
Cancer
Air Pollution
WeightLoss
Diabetes
Healthy Food
Health CareCost
Stress
Sodium
MentalHealthServices
BloodPressure
Trans fat
PrimaryCare
Cholesterol
Alcohol
Emergency Rehab Care
Sleep
Arthritis
4
PRISM Situates Multiple Medical, Behavioral, and
Environmental Factors into a Single Set of Causal
Pathways
5
PRISM Situates Multiple Medical, Behavioral, and
Environmental Factors into a Single Set of Causal
Pathways
6
PRISM Also Includes Frontiers for Social Action
Local Context for Weight Loss Services
Local Context for Tobacco
Local Context for Diet
Local Context for Physical Activity
Local Context for Air Pollution
Local Context for Health Care Services
Local Context for Mental Health Services
Secondhand
Air pollution
Smoking
Obesity
Excess
exposure
smoke
calorie diet
(PM 2.5)
Other deaths and costs
attributable to risk factors,
and costs of risk factor
Heart-
management
unhealthy diet
Chronic Disorders
-Hypertension
Uncontrolled
Cardiovascular
Total consequence
-High cholesterol
chronic disorders
Excess
events
costs
-Diabetes
sodium diet
CVD deaths,
disability,
Use of quality
and costs
preventive care
Physical
inactivity
Trans fat
Distress
consumption
7
Primary Information Sources
- Census
- Population, deaths, births, net immigration
- American Heart Association NIH statistical
reports - Cardiovascular events, deaths, and prevalence
- National Health and Nutrition Examination Survey
(NHANES) - Risk factor prevalence by age and sex
- Diagnosis and control of hypertension, high
cholesterol, and diabetes - Medical Examination Panel (MEPS), National Health
Interview (NHIS), Behavioral Risk Factor
Surveillance System (BRFSS), Youth Risk Behavior
Survey (YRBS) - Medical and productivity costs attributable to
risk factors - Prevalence of distress in non-CVD and post-CVD
populations - Primary care utilization
- Extent of physical activity
- Research literature
- CVD risk calculator (Framingham)
- Relative risks from secondhand smoke, air
pollution, obesity, poor diet, inactivity,
distress - Quality of diet (USDA Healthy Eating Index)
- Medical and productivity costs of cardiovascular
events - Effect sizes of behavioral interventions
- Expert judgment
Uncertainties are assessed through sensitivity
testing
8
Mapping Information SourcesPhysical Activity
Pathway
9
Mapping Information SourcesPhysical Activity
Pathway
10
Mapping Information SourcesPhysical Activity
Pathway
- Physical Inactivity Prevalence52 - 65 (by
age) - NHANES, BRFSS, YRBS
- Troiano RP, et al. Med Sci Sports Ex 2008
40(1)181-188.
11
Mapping Information SourcesPhysical Activity
Pathway
- Effective Interventions Increase PA by 40-55
(by age and strategy) - Kahn EB, et al. Am J Prev Med 2002 22S73-102.
12
Mapping Information SourcesPhysical Activity
Pathway
- RR for obesity onset 2.6
- Haapanen N, et al. Intl J Obesity 1997
21288-296
13
Mapping Information SourcesPhysical Activity
Pathway
- RR for distress 1.3
- Netz Y, Wu M-J, et al. Psyh Aging 2005
20(2)272-284. .
14
Mapping Information SourcesPhysical Activity
Pathway
- RR of inactivity if distressed 1.6
- Whooley MA, et al. JAMA 2008 300(20)2379-2388.
15
Mapping Information SourcesPhysical Activity
Pathway
- RR for High BP 1.15RR for High Cholesterol
1.4 - RR for Diabetes 1.4
- Ann Med 199123(3)319327.
- Intl J Epidemiology 1997 26(4)739-747.
- Canadian Med Assoc J 2000163(11)1435-1440.
- Lancet 1991 339778-783.
- Arch Intern Med 2001 1611542-1548.
16
Mapping Information SourcesPhysical Activity
Pathway
- Modification of theFramingham Risk Calculator
- Ex Rev Pharm Out Res 20066(4)417-24.
- Am Heart J 1991121(1 Pt 2)293-8.
- Am Heart J 2007153(5)722-31, 31 e1-8.
- JAMA 2001286(2)180-7.
17
Base Case Illustrative Intervention Scenarios
- Base Case (a simple scenario for comparison)
- Assume no further changes in the contextual
factors that affect risk factor prevalences - Any changes in prevalences after 2004 are due to
inflow/outflow adjustment process and
population aging - Result Past trends level off after 2004, after
which results reflect only slow adjustments in
risk factors - Increasing obesity, high BP, and diabetes
- Decreasing smoking
- Increases in risk factors and population aging
lead to eventual rebound in attributable deaths - Example Intervention Scenarios (max plausible
effects, sustained) - Four clusters of interventions layered to show
their partial contribution and combined effects - Services (health care, weight loss, smoking quit,
distress) Diet Physical Activity Tobacco
Air Pollution Sodium Trans fat
18
Illustrative Intervention Scenarios Maximum
Plausible StrengthIndividual Services Diet
PA Tobacco Air Pollution Sodium Trans fat
Smoking Prevalence (Adults)
Obesity Prevalence (Adults)
Draft Model Output
Draft Model Output
0.4
0.4
0.3
0.3
0.2
0.2
0.1
0.1
0
0
1990
2000
2010
2020
2030
2040
1990
2000
2010
2020
2030
2040
Cardiovascular Events per 1000(CHD, Stroke, CHF,
PAD)
Deaths from All Risk Factors per 1,000
30
Draft Model Output
Draft Model Output
8
22.5
6
15
4
7.5
2
0
0
1990
2000
2010
2020
2030
2040
1990
2000
2010
2020
2030
2040
if all risk factors0
Work in Progress, Please do no cite or distribute.
19
Illustrative Intervention Scenarios Maximum
Plausible StrengthIndividual Services Diet
PA Tobacco Air Pollution Sodium Trans fat
Years of Life Lost from Attributable Deaths
Consequence Costs per Capita (medical costs
productivity)
30 M
6,000
Draft Model Output
Draft Model Output
22.5 M
4,500
15 M
3,000
7.5 M
1,500
0
0
1990
2000
2010
2020
2030
2040
1990
2000
2010
2020
2030
2040
if all risk factors0
Work in Progress, Please do no cite or distribute.
20
Example of Sensitivity TestingEstimated impacts
of a 15-component intervention, with uncertainty
ranges
Total Consequence Costs per capita (2005 dollars
per year)
Deaths from CVD per 1000
3,000
4
Base Case
Base Case
2,000
2
Combined 15 interventions with range of
uncertainty
Combined 15 interventions with range of
uncertainty
1,000
Costs if all risk factors 0
Deaths if all risk factors 0
Model Output (v2008)
Model Output (v2008)
0
0
1990
2000
2010
2020
2030
2040
1990
2000
2010
2020
2030
2040
Homer J, Milstein B, Wile K, Trogdon J, Huang P,
Labarthe D, Orenstein D. Simulating and
evaluating local interventions to improve
cardiovascular health. Preventing Chronic
Disease, 2009 (in press).
21
How are Practitioners Using PRISM?
- A Few Local Versions
- Re-calibrate to areas with different
demographics, histories, and current conditions - Planning
- Engage a wider circle of stakeholders
- Situate silos within a system
- Prioritize interventions (given
tradeoffs/synergies) - Set plausible short- and long-term goals
- Evaluating
- Trace intervention effects through direct,
secondary, and summary measures - Extend the time horizon for evaluative inquiry
- Establish novel referents for comparison
(self-referential counter-factuals)
- Users (500)
- Customized Versions
- East Austin, Texas
- Mississippi Delta
- New Zealand Ministry of Health
- U.S. economic stimulus health initiative
- Natl State Stakeholders
- CDC Staff
- National Association of Chronic Disease Directors
- Directors of Public Health Education
- National Institutes of Health (NHLBI, OBSSR)
22
Conversations Around the Model
STRATEGIC PRIORITIES
- Whats in the model does not define whats in the
room - Simulations intentionally raise questions to
spark broader thinking and judgment - Narrower boundaries tend to be more empirically
grounded - Wider boundaries may legitimize invisible
processes - Boundary judgments follow from the intended
purpose and users
Local intervention opportunities and costs
Other health priorities
Community themes and strengths
SYSTEM DYNAMICS MODEL
Political will
Stakeholder relationships
Health inequities
Researchagenda
Available information
23
Interactive ModelingBuilds Foresight,
Experience, and Motivation to Act
Expert Recommendations
Experiential Learning Wayfinding