????????(CML) PowerPoint PPT Presentation
1 / 80
Title: ????????(CML)
1
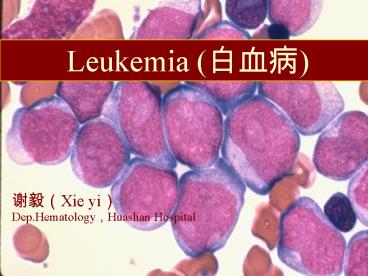
Leukemia (???)
??(Xie yi) Dep.Hematology,Huashan Hospital
2
Concept of leukemia
- Definition
- It is the results of the tumor proliferation of
heamotopoietic stem cells.(?????) - Leukemia is a malignant blood disorder. (not
solid tumor)
3
Heamatopoietic stem cell
- reproduction HSC
-
lymphoid HSC - HSC
- differentiation early
progenitor -
CFU-GEMM -
myeloid HSC - Heamatopoietic Stem Cell (HSC) is the primary
cell of Heamatopoietic system and immune system.
4
(No Transcript)
5
Tumor proliferation of HSC
- Differentiation of HSC is blocked.
- Leukemia cells are stopped on a differentiation
stage of HSC lack of the normal function . - Proliferation is out of control and apoptosis is
inhibited. - Leukemia cell is cloned and accumulated in a
great quantity. - infiltration and metastasis
6
malignant blood disorders
- HSC differentiation is blocked.
- Normal blood cells are decreased and leukemia
cell is increased. - The function of Blood and immune system are
short of. - Fever ,bleeding ,anemia
7
malignant blood disorders
- Proliferation is out of control ,apoptosis is
inhibited and leukemia cell is accumulated in a
great quantity. - Leukostasis(?????)
- Abnormal morphology pictures of blood and bone
marrow - Liver,spleen,lymph nods, skin,CNS are infiltrated
and dysfunctional frequently.
8
the tradition classification (FAB)of leukemia
- According to the acute myeloid leukemia(AML)
- Differentiation M0 M1 M2 .. M7
- Kind of cell blast crisis of CML,mast
cell leukemia, - acute eosinophilic
leukemia,basophilic - leukemia acute lymphocyte
leukemia(ALL) - L1,L2,L3
- T-ALL?B-ALL
- chronic leukemia CML?P-LL?CLL?HCL?
leukemia
9
WHO classification (2001)
- 1, Acute myeloid leukemia(AML)
- (1), AML with recurrent cytogenetic abnormalities
- AML with t(821)(q22q22),(AML1/ETO)
- AML with t(1517)(q22q12),(PML/RAR?)
- AML with inv(16)(p13q22) or
- t(1616)(p13q22) ,CBF?/MYH11
- AML with 11q23 (MLL) abnormalities
10
WHO classification (2001)
- (2), AML with multilineage dysplasia
- With prior myelodysplastic syndrome
- Without prior myelodysplastic syndrome
- (3),AML and myelodysplastic syndrome,
- therapy related
- Alkylating agent related
- Topoisomerase ll inhibitor-related
11
WHO classification (2001)
- (4) AML not otherwise categorized
- AML minimally differentiation
- AML without maturation
- AML with maturation
- Acute myelomonocytic leukemia
- Acute monoblastic and monocytic leukemia
- Acute erythroid leukemia
- Acute megakaryoblastic leukemia
- Acute basophilic leukemia
- Acute panmyelosis with myelofibrosis
- Myeloid sarcoma
- (5) Acute leukemia of ambiguous lineage
12
WHO classification (2001)
- 2, chronic myeloid leukemia
- (1), chronic myeloproliferative disease
- chronic myelogenous leukemia
- Chronic neutrophilic leukemia
- Chronic eosinophilic leukemia/hypereosinophilic
syndrome - (2), myelodysplastic/myeloproliferative disease
- Chronic myelomonocytic leukemia
- Atypical chronic myeloid leukemia
- Juvenile myelomonocytic leukemia
13
WHO classification (2001)
- 3, B-cell neoplasms
- (1), Precursor B-cell neoplasm
- Precursor B lymphoblastic leukemia
- (2), Mature B-cell neoplasm
- Chronic lymphocytic leukemia/Small lymphocytic
lymphoma (CLL/SLL) - B-cell prolymphocytic leukemia
- Hairy cell leukemia
- Burkitt lymphoma/leukemia
14
WHO classification (2001)
- 4, T-cell and NK-cell neoplasms
- (1), Precursor T-cell neoplasm
- Precursor T lymphoblastic leukemia
- (2), Mature T-cell and NK-cell neoplasms
- T-cell prolymphocytic leukemia
- T-cell large granular lymphocytic leukemia
- Aggressive NK leukemia/lymphoma
- Adult T-cell leukemia/lymphoma
15
Epidemiology incidence
- 3/105 , increase with years?
- acutegtchronic , AMLgtALL
- Special distribution
- Sex manfemale21
- Age ALL, adolescent 80lt20y AML, adult
- CML, 2050 years old CLL ,5070
years old - Area adult T lymphocytic leukemia
- CML, eastern countries
- CLL, western countries
16
Epidemiology mortality
- 2.51/105
- Area
- city gt the countryside
- ChinaltSingaporeltJapanltUSAltunited Kingdom
ltSweden(7.59/105) - In order of the mortality of malignant tumors
- in114y,leukemia is most high
- in1544y,leukemia is third high(ltstomach Calt
liver Ca) - in all person, leukemia is sixth or eighth high
17
Etiology
- radiation
- 1?atom bomb (? ?)1Km 1.5km 2km
- 100 22
2.6 - 2?high dose X radiation?32P therapy
18
Etiology
- chemicals
- benzene
- Therapy-related leukemia 47/440000
19
Etiology
- virus
- ATLV ,1981,Japan(???)
- electric microscopevirus C
- The serum antibody titer of ATLV
- decrease with the distance from ???
20
Etiology
- Genetics
- twin(same egg )
0.20.25 - sibling
10/105 - Downs syndrome (21) 40-60/105
Fanconi anemia
4/66
21
Etiology
- from other blood disorders
- Myeloproliferative Disease
- chronic myeloid leukemia(CML)
- polycythemia vera(PV)
- primary thrombocythemia(PT)
- myelofibrosis(MF)
- myelodysplastic syndrome(MDS)
- paroxysmal nocturnal hemoglobinuria(PNH)
- lymphoma or myeloma
22
Mechanism
- Radiation, chemicals, virus, genetics other
blood disorders - Chromosome translocation
- Fusion gene formation
- Fusion protein(enzyme )
- Malignant biologic behaviors
- Malignant blood disorders
23
Acute leukemia Clinical manifestation 1,
fever?bleeding?anemia 2?infiltration 3?Abnormal
morphology pictures of blood and bone marrow
24
1, fever?bleeding?anemia
- normal WBC??immune? ( AIDS) ?fever
- The place where skin and mucosa meet respiratory
tube, mouth, perineum, anus - Inflammatory reaction is weakly
- G-B(psuedomonas aeruginosa), interstitial
pneumonia (peumosystis arinii, CMV,herpes virus),
candida - PLT?? bleeding
- skin , mucosa or cranial cavity
- RBC?? anemia
25
2?infiltration
- Hepatomegaly, splenomegaly, lymphadenopathy,
- sternal tenderness
- Special infiltration area
- Chloromasskin ,orbit (granulocytic sarcoma)
- Painless enlargement of testicle( ALL)
- CNS involvement, paraplegia(ALL,M4,M5)
- gingivitis(M4,M5)
26
3?Abnormal morphology pictures of blood and bone
marrow
- Blood WBC from lt 1109/L(non leukemoid) to
gt100109/L ( hyperleukocytosis ), blasts are
present, anemia, PLT? - BMproliferative(or hypoplastic),blastsgt30,
Auers rods(), erythropoiesis ?,megakaryocytopoie
sis?
27
Normal bone marrow cell
28
leukemia cells ( show Auers rods )
29
Clinic Diagnosis of AL
- The normal blood cell?and luekemia cell?
- are shown by clinical signs, symptoms,
laboratory features and special examinations. - blast more than 30
- in non erythrocytic cells(NEC) of bone marrow
smear
30
MICM TYPING DIAGNOSIS
- MICM
- Morphology
- Immunology
- Cytogenetics
- Molecular
31
morphology
- lymphoblast myeloblast
monoblast - plasma ?,?? ?,Auers ?,???
- chromatin ?? ?? ?
- chromosome ?? ??
? - Accompany ??C, ?? ?? ??, ???
- POX - /??
-/?? - NSE - -/,NaF???
,NaF?? - PAS ??-?? ????? ????
32
IMMUNO-PHENOTYPING
- mab M1 M2 M3 M4 M5 M6 M7
- CD13 - -
- CD33 - -
- CD14 - - - -
- CD41 - - - - - -
- Ret - - - - - -
- Lectoferrin - - - - -
- CD19 CD7 HLA-DR CD2 MPO
- T - - -
- B - - -
33
Chromosome translocation
- M1 8,-5,-7 inv(3)
- M2 t(821) t(69)
- M3 t(1517)
- M4 inv(16)
- M5 t(411), t(816)
- M6
- M7
ALL t(922) (B) t(814)
34
Fusion gene molecular
- AML1/ETO
- PML/RAR?
- CBF?/MYH11
- MLL abnormalites
- BCR/ABL
35
MICM TYPING DIAGNOSIS
- We could use traditional typing diagnosis as what
FAB asked. - If the situation permit, we could use FCM,
chromosome, PCR or FISH in a WHO typing diagnosis
way.
36
Differential Diagnosis
- Myelodysplastic syndrome (MDS)
- refractory anemia or pancytopenia, BM
dysplasia, blastslt30 - Leukemoid reaction
- mature leukocytes proliferative would play a
main role, NAP?, if progenitor increase, only
shortly on time - CML mature progenitors ?
- E??B?, NAP0, ph'(),bcr-abl()
- Stomatitis,Infectious mononucleosis,ITP,
AA,agranulocytopenia - There is no blasts in bone marrow
37
principle early,combine,full,interval,by stages
- why early ?
- The over hyperplasia infiltration could bring
the difficulty on therapy - Tumor lysis
- Leukemia cell enter into the area protected by
the barrier between blood and brain - Could make anti-infection, support and
chemotherapy to be done at same time if it were
necessary
38
principle early,combine,full,interval,by stages
- use Combination regimen of these drugs which have
different action, - typing and toxicity
- to increase curative effect and decrease
toxicity
39
Different Action of Drugs
- ??? ???
- 6MP 6TG MTX ????
- ???
- MTX
HU - ?????
- VM26 Ara-C,CC
- ?????? DNA ?? ???,CCNU AMSA
- RNA DNA
- L-ASP VCR
,VM26 - protein ???DNA
- ??????,????,??,???,????
- ???CTX,??,BU,CB1348,CCNU,BCNU
VP16
40
Cell cycle and chemotherapy
G2
- end cell
- apoptosis
- Go (source of relapse)
- sensitive insensitive
M
S
G1
41
The drug typing
- CCSA CCNSA
- Antimetabolic drugs alkylating drugs
- S, 6MP, 6TG mustine,CTX,BU
- Ara-C, CC, MTX CB1348,CCNU
- HU, VP16 anthracycline antibiotics
- M, VCR, VDS, VM26 bleomycin A5(????)
- G1, L-ASP, prednisone harringtonine(???)
- G2, VP16
42
The drug s effect
- CCSA CCNSA
- effect
- dosage
dosage - the effect is increased by time the effect
increased by dosage
43
The toxicity of the drugs
- ??? ???? VCR ???
?? ??? - BM?? -
- - ??
- ????
- ????
- ??N?
- ??
- ????
- ???? v v v v
v v - ??????
- ??
44
principle early,combine,full,interval,by stages
- full
- the drug should work in all period of cell cycle
- the dosage should be full
- The regimen would be used repeatedly
- ,
Killing the cells in all period of cell cycle
repeatedly could make G0? cycle control the
source of relapse(MRD)
45
principle early,combine,full,interval,by stages
- Interval for 34 weeks before next therapy
- Leukemia cell
normal cell
- When get disease the greater part of cells
hyperplasia is inhibited - is not in G0 period
- easily killed by chemotherapy
in G0 period or not? - doubling time long
short - Recover in interval not easy to recover
easy to recover
46
principle early,combine,full,interval,by stages
Reduce MRD step by step Keep the DFS for long
time
- remission consolidation
maintenance - induction
- 10111012 1068
104(MRD) - prevent CNS leukemia
- 6 cycles 35years
47
(1) remission induction
- Regimen for ALL
- VP VCR 12mg
- (classical) NS 20cc V qw
- Prednisone 2030mg/d p.o
- use it till CR
- would be more effective,but relapse easily
48
Induction remission Regimen for ALL
- 1) VDLP
- VCR 12mgNS20cc V qw(1,8,15,21d)
- DNR 3040mg V gtt qd 13d, 1517d
- Pred 40mg60mg p.o 114d
- L-ASP 10,000u V gtt 19-28d
49
Induction remission Regimen for ALL
- 2) VP16 0.2 V gtt qd 3d
- Ara-C 0.10.15 V gtt qd7d
- MTX 23g V gtt 24h
- after 12h, leucovorin 69mg m q8h 2d
- hydrotherapy alkalize
- leukemia in CNS could be treated
50
Induction remission Regimen for ANLL
- HOAP(classical)
- VCR 12mg V
- harringtonine 14mg V gtt qd5-7d
- Ara-C 50-100mg V gtt Bid5-7d
- Prednisone 30-60mg p.o qd5-7d
- interval 14d
51
Induction remission Regimen for ANLL
- HA
- harringtonine 2-4mg V gtt7
- Ara-C 0.10.2 V gtt7
- HD Ara-C
- Ara-C 2.0 V gtt q12h3
- DA
- DNR 30 40mg V gtt3
- Ara-C 0.10.2 V gtt7
52
Induction remission Regimen for ANLL
- PML(M3) retinoid acid(ATRA)60-80mg p.o
- Use chemotherapy in consolidation stage
- When relapse As2O3 5mg V gtt28d
- Hypoplastic leukemia
- Ara-C 12.5mg M qd21d
- harringtonine 1mg M qd21d
53
CR
- there are not anemia fever hemorrhage and
infiltration - Hb gt100g/L WBC lt10109/L
- PLT gt100109/L
- BM blastslt5
54
(2)The regimen in consolidation remission stage
- Using a induction remission regimen for six
cyclesz - Using different induction remission regimen
alternately for six cycles
55
(3)maintenance remission regimen
- treatment with extended interval using the
different induction remission regimen alternately
for 35Y - in interval time the patients with ALL will take
CTX,6-MP,6-TG MTX, P.O - Not maintain therapy unless leukemia relapse
Protect the capacity of body immunity, improve
quality of life
56
supportive care
- conponent transfusion therapy
- RBC ,rhEPO
- platelet
- antibiotics(???),IVIG, rhG-CSF
- Vein high nutrition
- protect heart, liver kidney
57
others
- Therapeutic Leukapheresis
- To treat the Leukostasis (WBCgt105)
- To prevent tumor lysis syndrome
- immunotherapy
- monoantibody to CD33 drug
58
others
- Hemapoietic stem cell transplantation
- Could be curable
- Expensive and high risk
- Acute myelomonocytic leukemia with DIC
- Use the low molecular heparin to improve prognosis
59
CNS leukemia
- Incidence of ALL 10-40,ANLL 2-4
- Could be found in youth age, who
suffered from infiltration, easily
onset in remission stage always
60
The clinical manifestation diagnosis of
CNS leukemia
- Clinical examination
- Intracranial hypertension
- The signs of meninges stimulated
- the signs of nerves injure
- CSF examination
- presuregt200mmH20, sugar ?,protein(gt40mg/dl),WBCgt1
0/mm3 - could find leukemia cells
61
The treatment of CNS leukemia
- High dose MTX injection
- MTX 5-10mg sheath enjection Biw-qw
- (dilution with injection water 3ml,
add. dexamethasome 5mg) - 2.4Gy 60Co radiation to head
62
The prevention of CNS leukemia
- After CR
- MTX 5-10mg sheath rejection qw6
- Incidence of CNS leukemia?,lt5
63
Chronic Myelogenous Leukemia (CML)
- a Clonal proliferative disorder of pluripotent
stem cell - Consistently associated with the Ph chromosome
and BCR-ABL fusion gene - About 1525 of all cases of leukemia
- 2560 years, slightly more in men than women
64
MECHANISM Ph CHROMOSONE
65
MECHANISMPh CHROMOSONE
2
1
ABL
BCR-ABL Fusion gene
1 2 3
BCR
8.5Kb mRNA(b3a2 or b2a2)
210Kd protein(P210)
CML
7.5kb mRNA (b1a2) ? 190Kd(p190) ?Ph()ALL
66
CML development
- Initial indolent chronic phase(CML-CP,34
years)is followed by accelerated phase(CML-AP)and
blast phase(CML-BP,as acute leukemia)
67
Clinical manifestation
- Weight loss?fatigue ,excessive sweating
- sternal tenderness, splenomegaly
- WBC?
- gt200109/L, Leukostasis(?????)
68
Clinical manifestation
- WBC 101000109/L
- Granulocytes at all stages of development are
present in blood(??????) - or PLT gt1000109/L or anemia
- NAP(neutrophil alkaline phosphatase activity)0
- BM proliferate ?,Granulopoiesis is dominent .
blastlt10, B E? - ph1() 90 pcr, BCR/ABL fusion gene()
69
CML diagnosis
- Symptoms are vague and nonspecific
- Splenomagly,90sternal tenderness
- WBC 101000109/L
- Granulocytes at all stages of development are
present in blood, NAP0 - BM proliferate ?,Granulopoiesis is dominent
- blastlt10, B E? and Erythropoiesis ?
- megakaryocytopeoiesis ? and reticulin fibrosis ?
- ph1() ,bcr-abl ()
70
CML by stages
- Chronic phase accelerative phas blast
phase - Asymptomatic, anemia,hemorrhage, like as acute
- splenomegaly splenomegaly
leukemia - eosinophilia basophilic cell
- basophlia gt20
- blast blast
blast - lt 10 1020
gt20 - PLTlt100109/L
- gt 1000109/L
71
CMLdifferentiation diagnosis
- 1?leukemoid reaction
- infection,cancer etc
- WBC ? ,there isnt splenomegaly
- NAP ? ,absence of Blast, ph1, bcrabl
- 2?myelofibrosis
- WBC ? Splenomegaly
- teardrop poikilocytes,nucleared red cell in blood
- BMaspiration is often unsuccessful NAP ?
,absence of Blast, ph1 and bcrabl
biopsycollagen fibrosis
72
CMLdifferentiation diagnosis
- 3?acute leukemia
- ph1 in 2 AML
- ph1 in 525 ALL
- 4?acute abdomen
- Absence of splenomegaly and the fricative in left
hypochondrial region
73
CML treatment
- 1, keep WBC 4.010.0109/L
- (1) Hydroxyurea (???) 0.52.0 tid
- Busulfan (???)110mg qd
- ????????????????
- (2)Interferon a-2b 500?u H qd
- Ara-C 25mg H qd 1421?
- (3) Grivec (Greevec,??? ,STI 571 ) 400600mg/d
74
CMLs THERAPY
- 2, WBCgt200109/L, Leukostasis
- therapeutic luekopheresis
- 3, Blast Phase
- Like as acute leukemia , difficultly
- 4, Allo-BMT, Allo- PBSCT, CBT)
- curabale
75
Chronic lymphocytic leukemia(CLL)
- CLL is neoplastic disease
- The apoptosis of lymphocyte is inhibited
- Accumulation of small mature appearing CD5 B
lymphocytes in blood ,marrow and lymphoid tissues
- immunodeficiency
- incidence 20/ 105 in western country, 2/ 105 in
China - 90gt50y male female21
76
CLLdiagnosis
- 25 patients are asymptomatic
- Maybe nontender lymphadenopathy, splenomegaly and
hepatomegaly - Unexplained absolute lymphcytosis
- WBC 10200, lymphocytesgt 50, gt 5109/L (5000/mm3
) , gt4 weeks - BM lymphocytes gt40
77
CLLdiagnosis
- Lymphocyte surface immunologic marker can
determine monoclonality - immunophenotyping
- B,surface or cytoplasmic immunoglobuline , ? or
? light chains ,CD5 ,CD19 ,CD20
- T (fewer) ,CD2,CD3,CD8,CD5
78
CLL Rai staging diagnosis
-
median survival 0 L gt15109/L
gt150 month - I 0lymphadenopathy 105
- II Ispleno-hepatomegaly 71
- III IHb lt110g/L
19 - IV IPlt lt100109/L 19
79
CLLdifferentiation diagnosis
- With reactive lymphocytosis
- Mononucleosis syndrome
- Epstein Barr virus
- Cytomegalovirus
- HIV
- With other lymphoproliferative disorders
- Prolymphocytic leukemia, hairy cell leukemia,
lymphoma,Waldenström macroglobulinemia,
80
CLL therapy
- O observe, if WBC?, Lymphapheresis
- I / II Chlorambucil(CB1348),CB1348prednisone
- III / IV
- COP / Fludarabine(????)
- Cladribin ( 2-CdA ,2-?????)
- Pentostatin(Deoxycoformycin,??????)
- mabthera (CD20 mab,???), FCR regimen
- radiotherapy