Electronic Health Records (EHR) PowerPoint PPT Presentation
Title: Electronic Health Records (EHR)
1
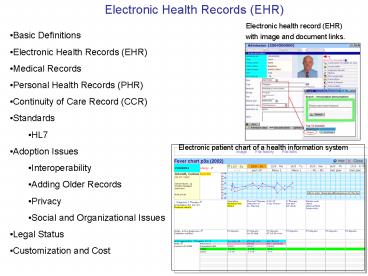
Electronic Health Records (EHR)
Electronic health record (EHR) with image and
document links.
- Basic Definitions
- Electronic Health Records (EHR)
- Medical Records
- Personal Health Records (PHR)
- Continuity of Care Record (CCR)
- Standards
- HL7
- Adoption Issues
- Interoperability
- Adding Older Records
- Privacy
- Social and Organizational Issues
- Legal Status
- Customization and Cost
Electronic patient chart of a health information
system
2
Electronic Health Records (EHR)
- An electronic health record (EHR) is a
distributed personal health record in digital
format. - The EHR provides secure, real-time,
patient-centric information to aid clinical
decision-making by providing access to a
patient's health information at the point of
care. - An EHR is typically accessed on a computer or
over a network. - It may be made up of health information from
many locations and/or sources, including
electronic medical records (EMRs). - An EHR almost always includes information
relating to the current and historical health,
medical conditions and medical tests of its
subject. - In addition, EHRs may contain data about medical
referrals, medical treatments, medications and
their application, demographic information and
other non-clinical administrative information. - The ideal EHR system, as of 2006, has not been
implemented by any software or other vendor.
3
Electronic Health Records (EHR)
- An electronic medical record (EMR) is a patient
medical record that contains both documents in an
electronic form and functions including - Patient demographics.
- Medical history, examination and progress reports
of health and illnesses. - Medicine and allergy lists, and immunization
status. - Scheduling, retrieval and archiving of laboratory
and other tests. - Graphic image display of X-rays, MRIs and other
medical imaging studies. - Medication ordering, including patient safety
functions to minimize interactions or
side-effects. - Evidence-based recommendations for specific
medical conditions, termed clinical practice
guidelines. - Appointment scheduling.
- Claims and payment processing.
- Patient reminders of follow up appointments, test
completion, preventive health practices.
4
Electronic Health Records (EHR)
- The electronic health record (EHR) is all patient
medical information from multiple sources,
including all components of the EMR, accessible
from any location by any provider caring for the
patient. - In this ideal, the information is continuously
updated and current. Terms commonly used in
describing the EHR include interactive,
interoperability, secure, real-time and
point-of-care. - The EHR allows collection of data for uses other
than for direct patient care, such as quality
improvement, outcome reporting, resource
management, and public health communicable
disease surveillance.
5
Medical Records
- A medical record is both a general term for an
individual's health documents and reports, or
more specifically, and often a paper chart or
folder containing this information. - Because of the need for access at different care
locations, a patient may have multiple medical
record folders at each location at which care or
testing was received. - Each record may contain partial information, and
the process of unifying and updating paper
records is daunting. - Handwritten reports or notes, manual order
entry, non-standard abbreviations and poor
legibility lead to medical errors, according to
the 1999 Institute of Medicine (IOM) report.
(Institute of Medicine (1999). To Err Is Human
Building a Safer Health System (1999). The
National Academies Press. Retrieved on
2006-06-20. ) - The follow-up IOM report advised rapid adoption
of electronic patient records, electronic
medication ordering, with computer- and
internet-based information systems to support
clinical decisions.
6
Medical Records (IOM report) http//books.nap.edu/
catalog.php?record_id9728
- Examples of Mistakes
- The knowledgeable health reporter for the Boston
Globe, Betsy Lehman, died from an overdose during
chemotherapy. Willie King had the wrong leg
amputated. Ben Kolb was eight years old when he
died during ''minor" surgery due to a drug
mix-up. - These horrific cases that make the headlines are
just the tip of the iceberg. - Two large studies, one conducted in Colorado and
Utah and the other in New York, found that
adverse events occurred in 2.9 and 3.7 percent of
hospitalizations, respectively. In Colorado and
Utah hospitals, 6.6 percent of adverse events led
to death, as compared with 13.6 percent in New
York hospitals. In both of these studies, over
half of these adverse events resulted from
medical errors and could have been prevented. - When extrapolated to the over 33.6 million
admissions to U.S. hospitals in 1997, the results
of the study in Colorado and Utah imply that at
least 44,000 Americans die each year as a result
of medical errors. - . More people die in a given year as a result of
medical errors than from motor vehicle accidents
(43,458), breast cancer (42,297), or AIDS
(16,516).
7
Personal Health Records (PHR)
- A personal health record is medical information
in possession of an individual patient or
patient's non-professional caregiver. - The format may be either paper documents,
electronic media, or a combination. The sources
of the information include patient-generated
lists, copies of reports from physicians,
hospitals and labs, legal documents such as
living wills and health care proxy forms, and
insurance statements. - Organizations such as the American Health
Information Management Association (AHIMA)
encourage individuals to keep their own complete
PHR, including any information that a doctor may
not have, such as exercise routines, dietary
habits, herbal or nonprescription medications, or
results of home testing, such as home blood
pressure or sugar readings. - Consumers can purchase PHRs from companies on the
internet. - According to AHIMA, 42 percent of US adults
surveyed said they keep some form of a personal
health record. PHR is also available free of cost
from several internet sites.
8
Personal Health Records (PHR) (cont)
http//www.myphr.com/
- Sample list of information gathered for patient
care - History and Physicaldescriptions of any major
illness and surgeries you have had, any
significant family history of disease, your
health habits, current medications, as well as
what your provider found when examining you. - Progress Notesnotes made by your healthcare
provider that reflect your response to treatment,
their observations, and plans for continued
treatment - Consultationopinion about your condition made by
a physician other than your primary care
physician - Physician's Ordersdirections to other members of
the healthcare team regarding your medications,
tests, diets, and treatments - Imaging and X-ray Reportsdescription of the
findings of x-rays, mammograms, ultrasounds, and
scans. - Lab Reportsdescription of the results of tests
conducted on body fluids. Common examples include
throat culture, urinalysis, cholesterol level,
and complete blood count - Operative Report--documentation that describes
surgery performed Pathology Reportdescription of
tissue removed during an operation and the
diagnosis based on examination of that tissue - Discharge Summarysummary of a hospital stay,
including the reason for admission, significant
findings from tests, procedures performed,
therapies provided, response to treatment,
condition at discharge, and instructions for
medications, activity, diet, and follow-up care
9
Continuity of Care Record (CCR)
- The Continuity of Care Record (CCR is a core data
set of the most relevant and timely facts about a
patient's healthcare. - It is to be prepared by a practitioner at the
conclusion of a healthcare encounter in order to
enable the next practitioner to readily access
such information. - It includes a summary of the patient's health
status (e.g., problems, medications, allergies)
and basic information about insurance, advance
directives, care documentation, and care plan
recommendations. It also includes identifying
information and the purpose of the CCR. - The CCR may be prepared, displayed, and
transmitted on paper or electronically, provided
the information required by this standard
specification is included. - However, for maximum utility, the CCR should be
prepared in a structured electronic format that
is interchangeable among electronic health record
(EHR) systems - .
- To ensure interchangeability of electronic CCRs,
this standard specifies that XML coding is
required when the CCR is created in a structured
electronic format. XML coding provides
flexibility that will allow users to prepare,
transmit, and view the CCR in multiple ways,
e.g., in a browser, as an element in an HL7
message or CDA compliant document , in a secure
email, as a PDF file, as an HTML file, or as a
word processing document. It will further permit
users to display the fields of the CCR in
multiple formats. . Equally important, it will
allow the interchange of the CCR data between
otherwise incompatible EHR systems.
10
Standards
- Although there are few standards for modern day
electronic records systems as a whole, there are
many standards relating to specific aspects of
EHRs and EMRs. - These include
- ASTM Continuity of Care Record - a patient health
summary standard based upon XML, the CCR can be
created, read and interpreted by various EHR or
Electronic Medical Record (EMR) systems, allowing
easy interoperability between otherwise disparate
enities.10 - ANSI X12 (EDI) - A set of transaction protocols
used for transmitting virtually any aspect of
patient data. Has become popular in the United
States for transmitting billing information,
because several of the transactions became
required by the Health Insurance Portability and
Accountability Act (HIPAA) for transmitting data
to Medicare. - CEN - CONTSYS (EN 13940), a system of concepts to
support continuity of care. - CEN - EHRcom (EN 13606), the European standard
for the communication of information from EHR
systems. - CEN - HISA (EN 12967), a services standard for
inter-system communication in a clinical
information environment. - DICOM - a heavily used standard for representing
and communicating radiology images and reporting - HL7 - HL7 messages are used for interchange
between hospital and physician record systems and
between EMR systems and practice management
systems HL7 Clinical Document
11
HL7 Standards
- Health Level Seven, Inc. (HL7), is an
all-volunteer, not-for-profit organization
involved in development of international
healthcare standards. - Headquartered in Ann Arbor, Michigan, U.S.,
Health Level Seven is a Standards Developing
Organization (SDO) that is accredited by the
American National Standards Institute (ANSI). - Founded in 1987 to produce a standard for
hospital information systems, HL7 is currently
the selected standard for the interfacing of
clinical data in most institutions . - HL7 and its members provide a comprehensive
framework (and related standards) for the
exchange, integration, sharing and retrieval of
electronic health information. - The standards, which support clinical practice
and the management, delivery, and evaluation of
health services, are the most commonly used in
the world
12
HL7 Standards (cont)
- The HL7 organization has grown from a 14 members
in 1987 to over 2200 members worldwide, including
500 corporate members today and international
affiliates in thirty three countries. - Collectively, they develop standards designed to
increase the effectiveness, efficiency and
quality of healthcare delivery - In fact, HL7s primary mission is to create
flexible, low-cost standards, guidelines, and
methodologies to enable the exchange and
interoperability of electronic health records. - Such guidelines or data standards are an
agreed-upon set of rules that allow information
to be shared and processed in a uniform and
consistent manner. - Without data standards, healthcare organizations
could not readily share clinical information. - Theoretically, this ability to exchange
information should help to minimize the tendency
for medical care to be so geographically isolated
and highly variable.
13
HL7 Standards (cont)
- Today HL7 standards development initiatives
include the following - standardization of knowledge representation
(Arden syntax) - specification of components for context
management (known as CCOW) - support for healthcare data interchange using
object request brokers - In distributed computing, an object request
broker (ORB) is a piece of middleware software
that allows programmers to make program calls
from one computer to another, via a network. - extend interoperability for the development of
Health Information Exchange - standardization of XML document structures
- The Extensible Markup Language (XML) is a
general-purpose markup language.1 Its primary
purpose is to facilitate the sharing of data
across different information systems. XML is a
generic framework for storing any amount of text
or any data whose structure can be represented as
a tree structure. This means that the text must
be enclosed between a root opening tag and a
corresponding closing tag. The following is a
well-formed XML document - ltbookgtGallia omnia divisa est in partes tres
.... lt/bookgt - specification of robust vocabulary definitions
for use in clinical messages and documents (cf.
SNOMED CT, LOINC) - SNOMED (Systematized Nomenclature of Medicine),
is a systematically organised computer
processable collection of medical terminology - functional specifications for an electronic
health record - work in the area of security, privacy,
confidentiality, and accountability.
14
Standards (cont)
- Architecture (CDA) documents are used to
communicate documents such as physician notes and
other material. - The HL7 Clinical Document Architecture (CDA) is
an XML-based markup standard intended to specify
the encoding, structure and semantics clinical
documents for exchange. - IHE - Integrating the Healthcare Enterprise
while not a standard itself, IHE is a consortial
effort to integrate existing standards into a
comprehensive best-practice solution - ISO - ISO TC 215 has defined the EHR, and also
produced a technical specification ISO 18308
describing the requirements for EHR
Architectures. - openEHR - next generation public specifications
and implementations for EHR systems and
communication, based on a complete separation of
software and clinical models.
15
Standards Organizations
- United States
- Not-for-profit organizations such as
- -the American Society for Testing and Materials
(ASTM) - -Health Level 7 (HL7) and Healthcare Information
and Management - -Systems Society (HIMSS) are
involved in the standardization process for
EHR in the United States. - -The Certification Commission for Healthcare
Information Technology (CCHIT) is a private
not-for-profit organization founded to develop
and evaluate the certification for EHRs and
interoperable health informatics networks. - International
- In Europe, CEN's TC/251 is responsible for EHR
standards - -while at a global level, ISO TC215 produces
standards for EHR requirements as well as
accepting certain standards from other standards
organizations. - -CEN/TC 251 works on compatibility and
interoperability between independent systems and
to enable modularity in Electronic Health Record
systems. - -The openEHR Foundation develops and publishes
EHR specifications and open source EHR
implementations, which are currently being used
in Australia and parts of Europe. - In Canada
- Canada Health Infoway (a private not-for-profit
organization started with federal government
seed money) is mandated to accelerate the
development and adoption of electronic health
information systems.
16
Adoption
- EHR issues
- As of 2006, adoption of EHRs and other health
information technology (HIT), such as computer
physician order entry (CPOE), has been minimal in
the United States. - Less than 10 of American hospitals have
implemented HIT - while a mere 16 of primary care physicians use
EHRs. - The vast majority of healthcare transactions in
the United States still take place on paper, a
system that has remain unchanged since the 1950s.
- The healthcare industry spends only 2 of gross
revenues on HIT, which is meager compared to
other information intensive industries such as
finance, which spend upwards of 10. - The following issues are behind the slow rate of
adoption - 1)Interoperability
- In healthcare, interoperability is the ability of
different information technology systems and
software applications to communicate, to exchange
data accurately, effectively, and consistently,
and to use the information that has been
exchanged.
17
Adoption (cont) Interoperability
The Center for Information Technology Leadership
described four different categories (levels) of
data structuring at which health care data
exchange can take place.
18
Adoption (cont) Adding of Older Records
- To attain the wide accessibility, efficiency,
patient safety and cost savings promised by EHR,
older paper medical records ideally should be
incorporated into the patient's record. - The digital scanning process involved in
conversion of these physical records to EMR is an
expensive, time-consuming process, which must be
done to exacting standards to ensure exact
capture of the content. - Because many of these records involve extensive
handwritten content, some of which may have been
generated by different healthcare professionals
over the life span of the patient, some of the
content is illegible following conversion. - The material may exist in any number of formats,
sizes, media types and qualities, which further
complicates accurate conversion. - In addition, the destruction of original
healthcare records must be done in a way that
ensures that they are completely and
confidentially destroyed. - Results of scanned records are not always usable
medical surveys found that 22-25 of physicians
much less satisfied with the use of scanned
document images than that of regular electronic
data.
19
Adoption (cont) Privacy
- A major concern is adequate confidentiality of
the individual records being managed
electronically. - According to the Los Angeles Times, roughly 150
people (from doctors and nurses to technicians
and billing clerks) have access to at least part
of a patient's records during a hospitalization,
and 600,000 payers, providers and other entities
that handle providers' billing data have some
access also. - Multiple access points over an open network like
the internet increases possible patient data
interception. In the United States, this class of
information is referred to as Personal Healthcare
Information (PHI) and access is regulated by the
Department of Health and Human Services (DHHS)
under the Health Insurance Portability and
Accountability Act (HIPAA) and local laws. - However, according to the Wall Street Journal,
the DHHS takes no action on complaints under
HIPAA, and medical records are disclosed under
court orders in legal actions such as claims
arising from automobile accidents. - HIPAA has special restrictions on psychotherapy
records, but psychotherapy records can also be
disclosed without the client's knowledge or
permission, according to the Journal.
20
Adoption (cont) Social and Organizational
Barriers
- According to the Agency for Healthcare Research
and Qualitys National Resource Center for Health
Information Technology, EHR implementations
follow the 80/20 rule - that is, 80 of the work of implementation must
be spent on issues of change management, - while only 20 is spent on technical issues
related to the technology itself. - Such organizational and social issues include
- restructuring workflows
- dealing with physicians' resistance to change
- creating a collaborative environment that fosters
communication between physicians and information
technology project managers. - Exemplifying this need are several highly
publicized HIT implementation fiascos, including
one at Cedars Sinai Medical Center in Los
Angeles, in which physicians revolted and forced
the administration to scrap a 34 million system.
21
Legal Status of EHRs
- Medical records, such as physician orders, exam
and test reports are legal documents, which must
be kept in unaltered form and authenticated by
the creator. - The individually defined Legal Health Record
(LHR) for each healthcare provider forms the
basis for response to subpoenas and other legal
processes that require evidentiary use of the
patient's 'medical record'. - Digital signatures Most national and
international standards accept electronic
signatures. - According to the American Bar Association. "A
signature authenticates a writing by identifying
the signer with the signed document. When the
signer makes a mark in a distinctive manner, the
writing becomes attributable to the signer. - With proper security software, electronic
authentication is more difficult to falsify than
the handwritten doctor's signature. - However, as the recent rise in identity theft
demonstrates, no security method can totally
prevent fraud, so auditing information security
will continue to be prudent when using EMR.
22
Customization and Cost
- Customization
- Pricing for Electronic Health Record (EHR)
systems is highly dependent on each practice's
unique needs. - Because every medical practice has distinct
requirements, systems usually need to be custom
tailored. - This is due to the majority of EHR systems being
based on templates that are initially general in
scope. - In many cases, these templates can then be
customized in co-operation with the
vendor/developer to better fit a medical
specialty, environment or other specified needs. - Cost
- In a 2006 survey by the Medical Records
Institute, lack of adequate funding was cited by
the 729 health care providers responding as the
most significant barrier to adopting electronic
records. - At the American Health Information Management
Association conference in October 2006, panelists
estimated that purchasing and installing EHR will
cost over 32,000 per physician, and maintenance
about 1,200 per month. - Hidden costs may also include office workflow
disruption during training or data re-entry
required by a new system, with fewer patient
visits and less income.
23
US medical groups' adoption of EHR (2005)
24
(No Transcript)
25
(No Transcript)
26
(No Transcript)
27
(No Transcript)
28
(No Transcript)
29
(No Transcript)
30
(No Transcript)
31
(No Transcript)
32
(No Transcript)
33
(No Transcript)
34
(No Transcript)
35
(No Transcript)