Syncope PowerPoint PPT Presentation
1 / 12
Title: Syncope
1
(No Transcript)
2
(No Transcript)
3
Syncope or Near Syncope
- Differential Diagnosis and Cost Effective Workup
4
Syncope
- Common reason to present to ER or to ambulatory
clinic - Transient loss of consciousness that is
accompanied by loss of postural tone - Due to transient hypoperfusion of the brain (from
numerous causes) - Near syncope?similar workup
- Rarely necessitates hospital admission
- Etiology broadly divided into three categories
- head, heart, and vessels
5
Head
- Primary neurologic events seizures (atonic
seizures, temporal lobe seizures, unwitnessed
grand mal seizures) - Psychiatric illness anxiety, panic attack,
conversion disorder - Neurally mediated events reflex mechanisms that
are associated with inappropriate vasodilatation,
bradycardia, or both. - --includes vasovagal, vasodepressor,
situational, carotid sinus syndrome
6
Heart
- Cardiac related events that cause a sudden drop
in cardiac output and therefore syncope - --tachyarrthymia (SVT, VT, torsades with long
QT) - --bradyarrythmias
- --PE (sizable)
- --atrial myxoma
- --ischemia
- --inability to increase cardiac output with
activity IHSS, aortic stenosis
7
Vessels (Orthostatic Hypotension)
- Medication related (antihypertensives, others)
- Autonomic insufficiency
- Dehydration/volume depletion
- Exaggerated physiologic response (hot tub
syncope, esp after EtOH) - Rare disordersAddisons, panhypopit, Shy-Drager
8
Workup Take home points
- Shot gun approach not helpful
- Patients remain undiagnosed in 34 of cases
- Most common to least common diagnosis
vasovagal, cardiac arrhythmia, orthostatic
hypotension, seizure - Therefore, directed (and thorough) history and
physical and an EKG can pinpoint the problem in
most cases
9
History
- What exactly was the patient doing (positional,
exertional, situational) - Any prodrome
- Postictal symptoms
- Medication history
- Interview family or witnesses
10
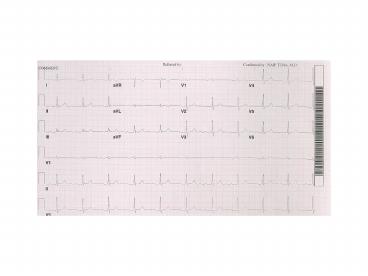
PE
- Check Orthostatic BP
- Cardiac exammurmur of AS/IHSS, tumor plop,
pulmonary HTN with RVH - Thorough neurologic exam
- EKG look for old infarcts, BBB, AV block
11
What about other tests?
- Labs rarely useful electrolytes may reveal low
K/Mg/Na/Ca, renal failure, or
hypo/hyperglycemia - These are rare to cause an event in and of
themselves, but can point to other etiology
(seizure) - Head CT, EEG only if focal neurologic findings
or if prior history of seizure - Carotid dopplers appropriate in the presence of
bruits or when the history suggests VBI
12
What if initial evaluation is negative?
- First, reassure patient (recall that a third
remain undiagnosed prognosis is generally good) - If suspected heart disease or risk factors for
heart disease echo, exercise stress test,
Holter monitor - Elderly patients same as above but consider
polypharmacy, situational syncope - Younger patients not known or suspected to have
heart disease ambulatory loop ECG, tilt table
testing, and psychiatric evaluation for
anxiety/panic disorder