Welcome to the PowerPoint PPT Presentation
1 / 73
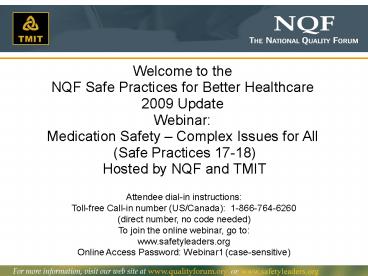
Title: Welcome to the
1
- Welcome to the
- NQF Safe Practices for Better Healthcare
- 2009 Update
- Webinar
- Medication Safety Complex Issues for All (Safe
Practices 17-18) - Hosted by NQF and TMIT
Attendee dial-in instructions Toll-free Call-in
number (US/Canada) 1-866-764-6260 (direct
number, no code needed) To join the online
webinar, go to www.safetyleaders.org Online
Access Password Webinar1 (case-sensitive)
2
Welcome and Overview of the Medication Management
Chapter of the 2009 NQF Safe Practices
Charles Denham, MD Chairman, TMIT Co-chairman,
NQF Safe Practices Consensus Committee Chairman,
Leapfrog Safe Practices Program Safe Practices
Webinar June 18, 2009
3
Panelists
Charles Denham
Peter Angood
Michael Cohen
Mary Andrawis
Patti ORegan
Jeffrey Schnipper
4
Culture SP 1
5
Culture
- CHAPTER 2 Creating and Sustaining a Culture of
Patient Safety (Separated into Practices - Leadership Structures Systems
- Culture Measurement, Feedback and Interventions
- Teamwork Training and Team Interventions
- Identification and Mitigation of Risks and Hazards
Culture Meas, F.B, Interv.
Structures Systems
ID Mitigation Risk Hazards
Team Training Team Interv.
Consent Disclosure
Consent Disclosure
- CHAPTER 3 Informed Consent Disclosure
- Informed Consent
- Life Sustaining Treatment
- Disclosure
- Care of the Caregiver
Informed Consent
Life Sustaining Treatment
Disclosure
Care of Caregiver
Work Force
- CHAPTER 6 Medication Management
- Medication Reconciliation
- Pharmacist Leadership Structures and Systems
- NEW
- Previous practices including Pharmacist Role,
High-Alert Medications, Standardized Medication
Labeling Packaging, and Unit-Dose Medications
are bundled into the Pharmacist Leadership
Structures and Systems practice. - Medication Reconciliation updated with expanded
Additional Specifications and Example
Implementation Approaches.
- CHAPTER 4 Workforce
- Nursing Workforce
- Direct Caregivers
- ICU Care
2009 NQF Report
Nursing Workforce
ICU Care
Direct Caregivers
Legend
- CHAPTER 5 Information Management Continuity of
Care - Critical Care Information
- Order Read-back and Abbreviations
- Labeling Studies
- Discharge Systems
- Safe Adoption of Integrated Clinical Systems
including CPOE
Information Management Continuity of Care
No Material Changes
Critical Care Info.
Labeling Studies
Material Changes
CPOE
Read-back Abbrev.
Discharge System
New
Medication Management
- CHAPTER 6 Medication Management
- Medication Reconciliation
- Pharmacist Leadership Role Including High-Alert
Med. Unit Dose Standardized Medication Labeling
Packaging
Med Recon.
Pharmacist Systems Leadership High Alert, Std
Labeling/Pkg, Unit Dose
- CHAPTER 7 Hospital Associated Infections
- UTI Prevention
- MDRO Prevention
- Care of the Ventilated Patient VAP,
- Central Venous Catheter Related Blood Stream
Infection Prevention - Surgical Site Infection Prevention
- Hand Hygiene
- Influenza Prevention
Healthcare Associated Infections
MDRO Prevention
UTI Prevention
VAP Prevention
Central V. Cath BSI Prevention
Sx Site Inf. Prevention
Hand Hygiene
Influenza Prevention
- CHAPTER 8
- Wrong Site, Wrong Procedure, Wrong Person Surgery
Prevention - Falls Prevention
- Organ Donorship
- Pressure Ulcer Prevention
- DVT/VTE Prevention
- Anticoagulation Therapy
- Gycemic Control
- Contrast Media-Induced Renal Failure Prevention
- Pediatric Imaging
Condition, Site, and Risk Specific Practices
DVT/VTE Prevention
Anticoag Therapy
Falls Prevention
Organ Donation
Pediatric Imaging
Wrong site Sx Prevention
Press. Ulcer Prevention
Contrast Media Use
Glycemic Control
6
Challenges of Policy Development for Medication
Management
Peter B. Angood, MD, FRCS(C), FACS, FCCM Senior
Advisor, Patient Safety National Quality
Forum Safe Practices Webinar June 18, 2009
7
Medication Safety Overview, Evolution, and
Current Issues
Michael Cohen, RPh, MS, ScD President, Institute
for Safe Medication Practices (ISMP) Safe
Practices Webinar June 18, 2009
8
Epidemiological ReviewIOM ? Preventing
Medication Errors
- Medications harm too many Americans
- At least 1.5 million people per year
- Hospitals
- 400,000 preventable ADEs per year
- About 1 medication error per patient per day
- Outpatient setting
- Also frequent, though data less solid
- 530,000 ADEs/year in Medicare patients
9
Event types reported to Pa-PSRS
10
Hospital Drug Distribution Systems
- Pre-1960s - floor stock system
- Locked narcotic safes/boxes (keys) with manual
counts - 1960s individual patient prescriptions
3-to-5-day supply, nurses poured own meds - 1970s unit-dose distribution IV admixtures
- Errors much more visible
- More pharmacist oversight of drug distribution
process - 1980s-90s Clinical pharmacy practice
- 1990s present - automated dispensing, robotics,
bar-coding, outsourcing for order review
11
Early Studies
Date Hospital Error Rate Observed
1962 University Florida 14.7
1964 University Arkansas 14.4
1967 University Kentucky (UD) 3.5
Kentucky Hosp A 8.3
Kentucky Hosp B 9.9
Kentucky Hosp C 11.5
Kentucky Hosp D 20.6
1975 Johns Hopkins 7.3
Johns Hopkins UD 1.6
12
Historic events in medication safety
Year Event
1960s-70s Studies show hospital ME rates up to 20 Community Pharmacy 3-5
1975 ME Feature in Hospital Pharmacy
1990 ISMP and USP form MERP
1992 Dateline NBC premieres with ME story
1995 Events in Florida, Massachusetts, Illinois all make headlines
1995 Leape, Bates, Cullen et al. JAMA
1996-7 IOM chartered study (To Err is Human)
1999 To Err is Human published
1999 TJC SE Alerts NPSGs Med Mgt Stds
2006 NQF Safe Practices Medication Management Chapter
2009 NQF Safe Practices Pharmacist Leadership Structures and Systems
13
Clinical consequences of a product-related error
14
(No Transcript)
15
(No Transcript)
16
(No Transcript)
17
Communication of Drug Information
- Look-alike/sound-alike drug names combined
with poor order communication, including during
digital transmission - Dangerous abbreviations and dose designations
- Suffixes misunderstood or omitted
- Confusion related to OTC brand name extensions
- Unsafe practices depicted in journal advertising
- Name confusion with medical terminology or
laboratory nomenclature - Same established name, different substance
internationally - More than one trademark for brand item
18
(No Transcript)
19
Use of mixed-case (tall-man) characters
- Dobutamine 400 mg
- Dopamine 500 mg
- chlorpropamide 100 mg
- chlorpromazine 100 mg
- hydralazine 50 mg
- hydroxyzine 50 mg
- doBUTamine
- doPAmine
- chlorproPAMIDE
- chlorproMAZINE
- hydrALAzine
- hydrOXYzine
20
Example of error due to lackof Patient
Information
21
Sound-alike
- Brand names
- FEMARA (letrozole) FemHRT
- SEROPHENE (clomiphene) and SARAFEM (fluoxetine)
- INVANZ (morphine extended release) or AVINZA
(ertapenem injection) - Nonproprietary names
- tamoxifen or tomoxetine (now atomoxetine)
- fomepizole or omeprazole
- torsemide or furosemide
Cohen MR. Medication Errors. Causes,
Prevention, and Risk Management 8.1-8.23.
22
Some changes to brand name as a result of
medication errors
- Losec (confused with Lasix) is now Prilosec
- Levoxine (confused with Lanoxin) is now Levoxyl
- Mazicon (confused with Mivacron) is now Romazicon
- Pediaprofen (confused with Pediapred) is now
Childrens Motrin - Altocor (confused with Advocor) is now Altoprev
- Reminyl (confused with Amaryl) is now Razadyne
- Omacor (confused with Amicar) is now Lovaza
23
Nonproprietary Name Changes
- amrinone or amiodarone (now inamrinone)
- tamoxifen or tomoxetine (now atomoxetine)
- fomepizole or omeprazole (fomepizole was
4-methylpyrazole 4-MP and concern was for
confusion with 6-MP mercaptopurine - torsemide or furosemide (torsemide was originally
torosemide)
24
Oral orders Read-back vs. Repeat-back
- The receiver of the order should write down the
complete order or enter it into a computer - Then the receiver should read it back
- Receive confirmation from the individual who gave
the order
25
(No Transcript)
26
Look-alike packaging
27
(No Transcript)
28
(No Transcript)
29
Lilly insulin color differentiation
30
United States Before and after both are same
strength
31
High-Alert Medications
- Small number of medications that have a high risk
of causing injury if misused - Errors may or may not be more common with these
than with other medications, but the consequences
of errors may be devastating
32
Leading Products in Harmful Medication Errors, CY
2005
Generic Name n
Insulin 386 11.3
Morphine 164 4.8
Heparin 120 3.5
Fentanyl 98 2.9
Hydromorphone 91 2.7
Warfarin 88 2.6
Potassium Chloride 69 2.0
Vancomycin 69 2.0
Enoxaparin 60 1.8
Metoprolol Tartrate 42 1.2
Furosemide 41 1.2
Methylprednisolone 35 1.0
Meperidine 33 1.0
MEDMARX annual report 2007
33
(No Transcript)
34
(No Transcript)
35
(No Transcript)
36
Medication Errors Reporting Program (MERP)
- Operated by theUnited States Pharmacopeia
- in Cooperation with theInstitute for Safe
Medication Practices - www.ismp.org
Pennsylvania Patient Safety Reporting Program
ISMP is a federally certified Patient Safety
Organization
37
Actionable Items
- Be proactive, not reactive. Learn from experience
of other organizations. Medication safety
officer/team. - Focus on unsafe practices/at risk behaviors
(e.g., unlabelled containers, sharing insulin
pens, abbreviating drug names, patient weight
conversions, etc.) - Implement technologies (smart pumps, bedside
bar-code scanning, follow automated dispensing
cabinet guidelines, e-Rx, etc.) - Standardize drug concentrations, units of
measure, etc. - Encourage error reporting internal and external
(see ISMP Med Safety Alert! Pump up the volume
tips for increasing reporting. Feb 9, 2006 )
http//www.ismp.org/Newsletters/acutecare/articles
/20060209.asp
38
Perspectives on the Importance of the Pharmacist
Leadership Safe Practice in the Hospital
Environment
Mary Andrawis, PharmD, MPH Director, Clinical
Guidelines and Quality Improvement American
Society of Health-System Pharmacists (ASHP) Safe
Practices Webinar June 18, 2009
39
The Pharmacists Mission
- To help patients make the best use of medicines
- Extensively trained to ensure safe and
evidence-based use of medications - Expanded role to meet the need for comprehensive
medication management
40
Literature clearly demonstrates improved patient
outcomes, fewer adverse events, and reduced costs
when pharmacists are involved in care.
41
Safe Practice 18 Pharmacist Leadership
Structures and Systems
Pharmacy leaders should have an active role on
the administrative leadership team that reflects
their authority and accountability for medication
management systems performance across the
organization.
42
Health-System Administrative Team
Pharmacy Leader
43
Items of Impact on Care
- Organizational decision-making.
- Involve pharmacy leaders with
- integral system decisions.
- Direct communication. Engage pharmacy leaders
with the organizations leadership team and the
Board.
ASHP Statement on the Roles and Responsibilities
of the Pharmacy Executive PDF
44
Items of Impact on Care
- Medication Safety Committee. Create a committee
led by pharmacy leaders to review errors. - Walk-rounds. Evaluate
- medication processes and
- get front-line staff input on
- medication safety.
ASHP Guidelines on Preventing Medication Errors
in the Hospital PDF
45
Items of Impact on Care
- Technology Readiness Planning. Call on pharmacy
to play central role in planning and
implementation of technologies that affect
medication use.
ASHP Statement on Bar-Code-Enabled Medication
Administration Technology PDF
46
Items of Impact on Care
- Pharmacists on Clinical Teams. Place clinical
pharmacists on rounds to optimize safe and
evidence-based selection and monitoring of
medications.
ASHPSHM Joint Statement on HospitalistPharmacist
Collaboration PDF
47
- Utilize your pharmacy leaders to get
- better patient outcomes
- fewer medication errors, and
- lower costs.
- Examples of Pharmacists Impact
48
Where the Rubber Meets the Road Implementation
of Medication Reconciliation at the Practitioner
Level
Jeffrey Schnipper, MD, MPH, FHM Director of
Clinical Research, BWH Hospitalist Service
Associate Physician, Division of General
Medicine, Brigham and Women's Hospital Assistant
Professor of Medicine, Harvard Medical
School Safe Practices Webinar June 18, 2009
49
Goals of This Talk
- To review the experience at Partners regarding
medication reconciliation - Which patients are at highest risk
- Benefits of Health Information Technology-based
solutions - Other lessons learned
- To discuss various ways to approach solutions for
medication reconciliation
50
Classifying and Predicting Errors of Inpatient
Medication Reconciliation
Jennifer R. Pippins, MD, Tejal K. Gandhi, MD,
MPH, Claus Hamann, MD, MS, Chima D. Ndumele, MPH,
Stephanie A. Labonville, Pharm D, BCPS, Ellen K.
Diedrichsen, Pharm D, Marcy G. Carty, MD, MPH,
Andrew S. Karson, MD, MPH, Ishir Bhan, MD,
Christopher M. Coley, MD, Catherine L. Liang,
MPH, Alexander Turchin, MD, MS, Patricia
McCarthy, PA, MHA, and Jeffrey L. Schnipper, MD,
MPH J Gen Intern Med 200823(9)1414-22
51
Effect of a Medication Reconciliation Application
and Process Redesign on Potential Adverse Drug
Events A Cluster-Randomized Trial
- Jeffrey L. Schnipper, MD, MPH, Claus Hamann, MD,
MS, Chima D. Ndumele, MPH, Catherine L. Liang,
MPH, Marcy G. Carty, MD, MPH, Andrew S. Karson,
MD, MPH, Ishir Bhan, MD, Christopher M. Coley,
MD, Eric Poon, MD, MPH, Alexander Turchin, MD,
MS, Stephanie A. Labonville, Pharm D, BCPS, Ellen
K. Diedrichsen, Pharm D, Stuart Lipsitz, ScD,
Carol A. Broverman, PhD, Patricia McCarthy, PA,
MHA, and Tejal K. Gandhi, MD, MPH - Arch Intern Med 2009169(8)771-80
52
Specific Aims
Determine the effects of a redesigned process for
medication reconciliation, supported by
information technology, on unintentional
medication discrepancies with potential for
patient harm (potential ADEs)
53
Intervention I PAML Builder
54
PAML Builder Action on Admission
55
Reconciliation at Discharge (Site 1)
56
Description of Intervention II Process Re-design
- Admission
- Ordering physician takes medication history,
creates PAML - Nurse confirms accuracy of PAML
- Physician chooses planned action on admission,
writes admission orders - Pharmacist reconciles PAML and admission orders
- During Hospitalization
- PAML updated during hospitalization as needed
- Discharge
- Physician reviews PAML and current medications,
creates discharge orders, documents
reconciliation - Nurse reconciles PAML, current medications, and
discharge medications, reviews discharge
medications with patient/caregiver
57
Medication Reconciliation Errors in the Control
GroupN180
58
PADE Risk Score
Gout medications, muscle relaxants,
hyperlipidemic medications,antidepressants,
respiratory medications
59
Distribution of PADE Risk Scores
60
Results of RCT
Outcome Events, N (per patient) in Usual Care Events, N (per patient) in Intervention Adjusted and Clustered RR (95 CI)
All PADEs 230 (1.44) 170 (1.05) 0.72 (0.52-0.99)
PADEs due to History Errors 153 (0.96) 125 (0.77) 0.80 (0.55-1.15)
PADEs due to Reconciliation Errors 80 (0.50) 52 (0.32) 0.62 (0.29-1.34)
PADEs at Admission 49 (0.31) 44 (0.27) 0.87 (0.51-1.52)
PADEs at Discharge 181 (1.13) 126 (0.78) 0.67 (0.49-0.98)
61
Subgroup Analyses
Subgroup N Adjusted RR (95 CI) P value for interaction
SiteSite 1Site 2 170152 0.60 (0.38-0.97)0.87 (0.57-1.32) 0.32
PADE Risk Score0-3 points4-7 points 155167 1.09 (0.49-2.44)0.62 (0.41-0.93) 0.02
62
Discussion
- Intervention successful
- NNT 2.6 to prevent one PADE
- Effective combination of IT and process redesign
- But potentially harmful medication discrepancies
remained - Incomplete/inaccurate medication sources
- Lack of patient/caregiver knowledge of
medications - Lack of clinician adherence with process
- Software usability issues
63
Discussion
- Why more successful at Site 1 than Site 2?
- Differences in timing of roll-out, publicity
- Greater involvement of nurses
- Software integration at discharge
- Chance
64
Reconciliation at Discharge (Site 1)
65
Reconciliation at Discharge (Site 2)
66
Implications
- Unintentional medication discrepancies with
potential for patient harm are very common - Most are due to history errors
- Most occur at discharge
- Most are due to omissions
- Patients at high risk can be identified
- Low understanding of preadmission medications
- Number of total and high-risk preadmission
medications - Frequent outpatient visits
- Efforts need to focus first on taking accurate
medication histories, second on correcting
reconciliation errors at discharge
67
Implications (contd)
- Rigorous evidence that medication reconciliation
can benefit patients - Particular benefits of IT tools
- Ability to use existing electronic sources of
ambulatory medication information - Better workflow integration in sites with CPOE
- Easier sharing of information across providers
- Automatic production of discharge documentation
- Comparisons of medication lists to facilitate
reconciliation and patient education - Provision of alerts and reminders to ensure
compliance - Ability to track compliance to inform QI
68
Discussion
- Steps Taken to Improve Intervention
- Incomplete/inaccurate medication sources
- Working on Link to SureScripts/HubRx Data
- Post-discharge medication reconciliation so EMR
list is more accurate next time - Lack of patient/caregiver knowledge of
medications - Patient education
- Lack of clinician adherence with process
- Cannot write orders if PAML not complete within
24 hours of admission continued education
culture change with time - Better utilization of pharmacists (help with
history rather than police of admission order
discrepancies) - Software usability issues
- Better integration with admission orders
- Improvements to discharge screens still to come
69
Approaches to Medication Reconciliation
- Pharmacists take medication histories, confirm
reconciliation at admission and discharge in
all patients - Likely most effective the most successful
interventions in the literature have had
extensive pharmacist involvement - Also the most resource intensive
- Pharmacist technicians take medication
histories in the Emergency Department (e.g.,
Novant Health) - Physicians take medication histories in most
patients, pharmacists play supporting role in
most patients reserve greater pharmacist
involvement for high-risk patients
70
Conclusions
- Medication reconciliation can work
- HIT can be part of the solution
- Interdisciplinary communication is key
- Focus should be on taking good medication
histories and reconciling medications at
discharge - With HIT, little usability issues mean a lot
- Collectively, we need access to better sources of
preadmission medication information - Patients and caregivers need to be more a part of
the solution - Several approaches to use of personnel are
possible not clear which is most effective and
efficient
71
Patient Perspective on Medication Management Safe
Practices
Patti ORegan, ARNP, ANP, NP-C, PMHNP-BC Nurse
practitioner, Port Richey, FL founding member,
TMIT Patient Advocate Panel Safe Practices
Webinar June 18, 2009
72
Panelists
Charles Denham
Peter Angood
Michael Cohen
Mary Andrawis
Patti ORegan
Jeffrey Schnipper
73
Upcoming Safe Practices Webinars
- July 16 Leadership and Leadership Principles
for Safety (Safe Practices 1-4) - September 17 Important Condition and Common
Safety Issues (Safe Practices 26-34) - October 22 Creating Transparency, Openness, and
Improved Safety (Safe Practices 5-8) - November 19 Healthier Communication and Safe
Information Management (Safe Practices 12-16) - December 17 Optimizing a Workforce for Optimal
Safe Care (Safe Practices 9-11)