ILIOTIBIAL BAND SYNDROME (ITB) - PowerPoint PPT Presentation
Title:
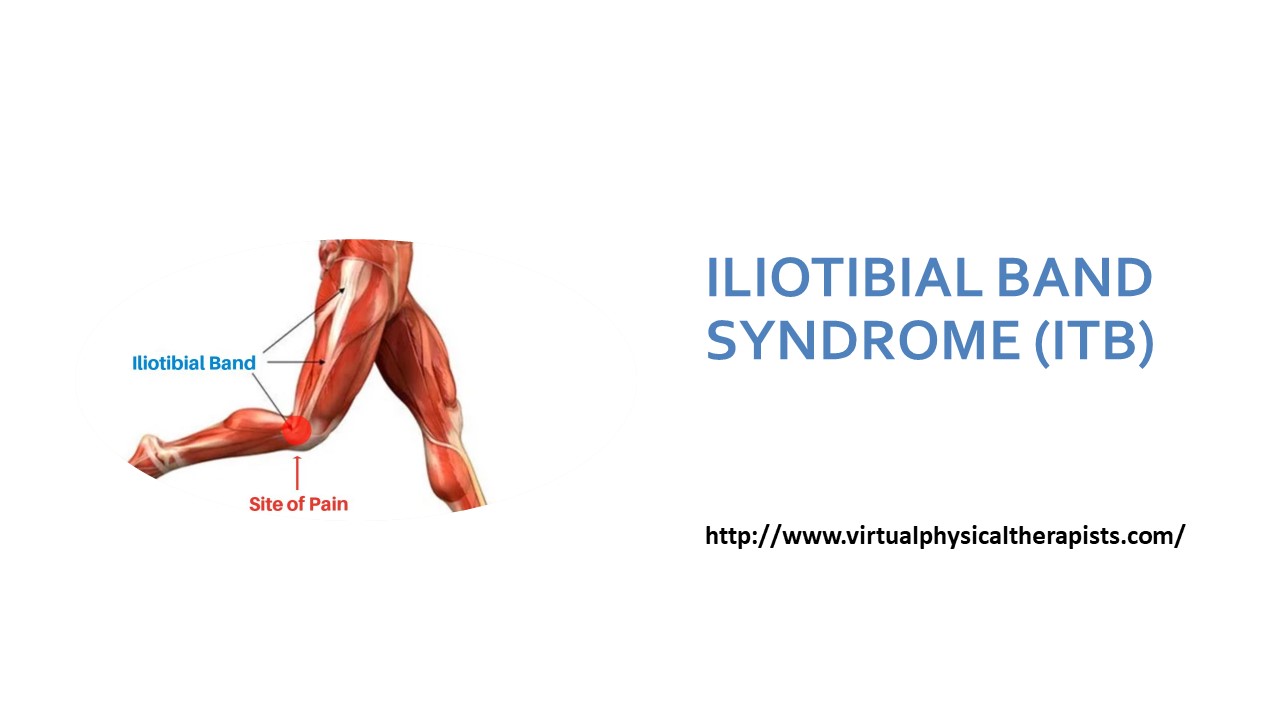
ILIOTIBIAL BAND SYNDROME (ITB)
Description:
Iliotibial band (ITB) syndrome is one of the most common overuse injuries in runners. Virtual physical therapy helps runners identify the biomechanical issues of ITB and educates them with knowledge about the causes of iliotibial band syndrome, biomechanics, causes of pain, misdiagnosis, rehabilitation, prevention, and more. – PowerPoint PPT presentation
Number of Views:5
Title: ILIOTIBIAL BAND SYNDROME (ITB)
1
ILIOTIBIAL BAND SYNDROME (ITB)
http//www.virtualphysicaltherapists.com/
2
Iliotibial band (ITB) syndrome is one of the most
common overuse injuries in runners. It is also
seen in cycling and other activities that require
repetitive bending of the knee. Treatment must
focus on eliminating the causative factors.
Virtual Physical Therapy can help identify
biomechanical issues and educate you on how you
can get back to running pain-free!
3
- ITB syndrome usually starts suddenly as
discomfort or even burning on the outside of the
knee. It can quickly turn into a sharp pain and
quickly progress to a feeling of a vice around
your knee that gets tighter and tighter until the
pain stops you from moving. Initially, the
symptoms are only brought on by aggressive
activity such as running and cycling but as they
progress, sitting with your knee flexed becomes
unbearable, requiring straightening of the knee
to release pressure.
4
What Causes Iliotibial Band Syndrome? The number
one cause is too many miles! Minor issues with
running mechanics become exacerbated when
fatigued, and your muscles are weakened from
overtraining. Not allowing your body time to heal
leads to poor mechanics, tears in soft tissue,
damage. In the case of ITB syndrome it is due to
irritation and thickening of a fat pad over the
femoral epicondyle that the ITB repetitively
compresses. Banked surfaces (always running in
the same direction as road camber) and downhill
running (eccentric muscle control gives way
faster when fatigued) can cause increased stress
and compression of the ITB.
5
Anatomy
- The ITB is a thick fibrous band extending from
above your hip to below your lateral knee. The
proximal portion begins as a sheath encasing the
tensor fascia lata muscle. This sheath anchors
the tensor fascia lata to the iliac crest and
receives most of the superior gluteus maximus
tendon. The dense ITB then extends all the way
down the lateral leg and transitions to a
ligamentous component, spanning from the lateral
epicondyle of the femur (just above the outside
knee) to five insertion points distally including
the knee capsule and Gerdys tubercle just below
the lateral knee.
6
- Biomechanics
- The ITB acts as both a stabilizer for the hip and
knee as well as elastic energy during walking and
running. It is a distinctive tissue in that it
has some properties of a tendon but most of a
ligament. It is also unique because humans are
the only mammal to have one. It is theorized that
the ITB aids in our ability to stand on one leg
and walk upright and is not needed in 4 legged
mammals. We are not born with a distally
inserting ITB, but rather developed as we learn
to walk. - The iliotibial band transmits the forces
generated by the TFL and gluteus maximus muscles,
including thigh abduction, flexion, extension,
and external rotation. The deep fascial
component, which runs almost the entire femur
length, is most taut when the gluteus maximus and
TFL contract. This tensile action significantly
increases during single-leg stance and serves to
counteract medial bowing of the femur.
7
- The ITB is actually a ligament/tendon hybrid
because it has a bone-to-bone connection as seen
in ligaments and muscle-to-bone connections as
found in tendons. The ITB is NOT anchored to a
bone at a clear, specific spot like most tendons.
Instead, it blends into five different areas
distally including the knee capsule. Tendons are
smaller, dense connective tissue at the end of
the muscle. The ITB, on the other hand, connects
the muscles by a very thin sheath and is massive
compared to the muscles it connects. - The gluteus muscle pulls on the ITB to increase
its tension laterally, like drawing a bowstring.
It is then tightly anchored along the entire
length of the femur, especially above the knee.
The ITB does not really move freely in relation
to the femur. It is firmly attached. The only
slight movement may be at the insertion at
Gerdys tubercle, just below the lateral knee.
8
- Cause of Pain
- Iliotibial band syndrome occurs secondary to
repetitive compression. Faulty mechanics caused
an increase in compression at the distal end of
the ITB as the hip extends and the knee flexes.
The bony prominence of the lateral epicondyle has
a protective synovial tissue or fat pad. This
synovial tissue can become irritated, thickened,
and even calloused. Once calloused, it can be
felt like rubbing over a rubber band.
9
- For many years it was believed that the pain was
due to friction of the ITB over the lateral
femoral epicondyle. The ITB is tethered to the
distal femur, except for the upper portion of the
lateral femoral condyle, preventing movement of
the ITB across the lateral femoral condyle. - Biomechanics that cause an increase in the
compression of the ITB include genu varum (knees
go inward), increased pronation, and hip
weakness. These are in opposition to the role of
the ITB, to pull on the femur laterally like a
bowstring. - The main problem and symptoms occur at 30 deg of
knee flexion with the hip in slight extension
this is when the ITB is mostly clamped down.
10
- Misconceptions
- 1. The ITB is the painful structure. The painful
tissue is underneath the ITB. It is synovium or
tissue similar to a fat pad that is a lateral
extension of the knee capsule. Repetitive stress
causes it to become callused, and it gets
pinched. Occasionally there can also be
calcified loose bodies if the stress on this
synovial tissue continues. - 2. The ITB needs to be stretched using a foam
roller or specific stretching. The ITB is mostly
a ligament in structure. The role of a ligament
is to maintain a taunt attachment to bone. You do
not want loose ligaments as this leads to
instability. The ITB is also a vast thick
structure similar to a thick leather belt. You
can pull on it all you want, and it still will
not stretch. Foam rolling adds more compression
to a tissue that has been already irritated by
compression.
11
- 3. Corticosteroid injections causes local cell
death and tendon atrophy! Steroids have an
important place in medicine but must be used with
caution. Inflammation is part of the bodys
natural healing process, and when it is
terminated, it disrupts healing and can lead to
tendon damage. The main treatment focus should be
addressing the actual cause of ITB syndrome or
repetitive stress/compression causing the tissue
to become calloused.
12
- Running
- Humans are built for running, and we may even be
one of the best species for long-distance. Every
year in Wales, there is an endurance race of
humans against horses, and believe it or not,
humans won twice because of hot conditions. If we
are built for running, then why do we get so many
injuries? Its because of poor mechanics and our
training.
13
- Running
- Humans are built for running, and we may even be
one of the best species for long-distance. Every
year in Wales, there is an endurance race of
humans against horses, and believe it or not,
humans won twice because of hot conditions. If we
are built for running, then why do we get so many
injuries? Its because of poor mechanics and our
training.
14
- Mechanism of Injury
- The ITB is most taunt when the hip is extended
and the knee is flexed to 30 degrees. The hip
goes into extension during the swing phase of
running when the knee bends. Severe symptoms
almost completely abolish as soon as the
individual stops walking because the hip does not
extend in walking. The faulty mechanics found in
those that suffer from ITB on the painful side
include - 1. Hip drops down and in (adducts)
- 2. Ankle bone drops down and in (pronation)
during heel strike - 3. Heel is inward during the swing phase.
15
- The faulty mechanics are exacerbated with fatigue
as the muscles tire leading to weakness in hip
abduction weakness causing the hip to drop inward
and tibialis anterior fatigue causing pronation
of the foot. Road cadence constantly running on
one side of the road places uneven stress on the
leg, and poor footwear can cause increased
pronation.
16
- Physical Evaluation
- 1. A good clinician will first RULE OUT the
lumbar spine. There is a high incidence of
isolated extremity symptoms originating from the
spine. Therefore the spine must always be
screened. This is easily done by moving the spine
to see if it has any effect on the symptoms of
complaint along the outer knee. - 2. Observation Screen for alignment and any
abnormalities - 3. Palpation Assess for any tenderness and
palpable bursa along the lateral femoral
eopicondyle. - 4. Test for ITB Syndrome Have the individual
repetitively flex and extend the knee with hip in
extension. A positive test is the reproduction of
lateral knee pain. - 5. Muscle strength (hip abduction, external
rotation, quad, foot) - 6. Flexibility quad, hamstring, calf, and soleus
- 7. Gait/running assessment
17
- Rehabilitation
- Active REST
- An initial rest from running in favor of another
aerobic activity cycling, swimming, etc. so
activity can continue while eliminating
compression over the lateral epicondyle.
Gradually return to running (initially avoid
downhill) 3 days to 6 weeks depending on the
individuals symptoms. Average avoidance of
running 1 week. (2-6 months until recovery is
complete) - Address limitations
- Full quad, hamstring, and calf flexibility
- Improve hip, knee, and foot strength
18
- Address running mechanics
- Land with ankle bone high
- Swing phase with heel out
- Return to running
- Faster, shorter runs initially (Slow running
causes increased pressure on ITB. Sprinting
reduces compression.) - Adjust running style shorter stride and lower
(initially) - Avoid downhill
- Gradually increase millage
19
- Prevention
- Learn proper running mechanics (GOATA). Schedule
an assessment with one of our GOATA specialists. - Training!!!! Gradual increase in millage
- Maintain adequate strength and flexibility
- Avoid always running on one side of the road if
there is camber
20
Virtual physical therapists
- info.virtualphysicaltherapists_at_gmail.com
- http//www.virtualphysicaltherapists.com/