The Cardiovascular System PowerPoint PPT Presentation
1 / 37
Title: The Cardiovascular System
1
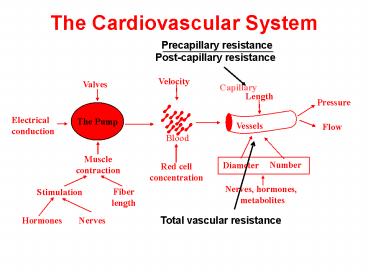
The Cardiovascular System
The Pump
2
Multifactorial control of the peripheral
vasculature
3
COMPETING DEMANDS
- The cardiovascular system is organized to respond
to multiple demands simultaneously, and
especially to meet crises. Responses are
mediated by multiple mechanisms. - Intrinsic mechanisms regulate capillary flow and
pressure of each organ. - Extrinsic mechanisms, nerves and hormones
coordinate functional needs of the organism as a
whole. - Bleeding causes neurally mediated constriction of
most vascular beds. - Generalized vasoconstriction helps to sustain
blood pressure, and improves cardiac function. - In the heart and striated muscle, intrinsic
mechanisms can over ride the vasoconstrictor
signals to allow the muscles to do the work of
escaping from the big cat
4
COMPETING DEMANDS
- Much of vascular physiology is organized to
protect the brain in times of crisis. - For example, the brain vasculature is protected
from most vasoconstrictor stimuli by the
blood-brain barrier. - Furthermore, in times of crisis, the vascular
function of all organs will be sacrificed to
maintain the cerebral blood flow and to permit
the animal (or person) to escape.
5
VASCULAR SMOOTH MUSCLE (VSM)
VSM is capable of graded contraction, i.e.,
contraction is not all-or- nothing. This
means that vascular diameter can be precisely
controlled by graded contractions and
relaxations of the smooth muscle. Contractile
strength is determined by the level of
intracellular calcium and the degree of myosin
phosphorylation. Ca sources include
extracellular fluid, inner cell membrane, and
sarcoplasmic reticulum.
6
The VSM intracellular Ca can be modulated by
- Membrane potential causing opening of L-type or
T-type Ca channels - K modifies smooth muscle contraction by changing
in membrane potential - Release of Ca from intracellular stores.
- norepinephrine can act directly on intracellular
stores - Phosphorylation of contractile proteins,
channels, pumps, and IP3 receptors can all be
modified by - Myosin kinases and phosphatases
- Regulated by cyclic AMP and cyclic GMP
7
VSM commonly manifests tone - a state of partial
contraction.
- All dilators work to reduce tone. Tone may be
either - Spontaneous - that is an inherent property of the
muscle cells, perhaps due to a relatively high
leak of Ca - Induced - resulting from exposure to stimuli
- Agonist induced, e.g. norepinephrine from the
nerve terminals - Stretch induced the response to stretch is
often referred to as the myogenic response. - see autoregulation below
8
SMOOTH MUSCLE - ENDOTHELIAL CELL COOPERATION
- The smooth muscle effect is terminated by
phosphodiesterase 5 - removes the cGMP and allows intracellular Ca
to rise - Viagra (sildenafil) works by inhibiting
phosphodiesterase5. - Unfortunately nitro-vasodilators (e.g.
nitroglycerine) also work by - elevating cGMP. The combined effect of
Viagra and nitroglycerine can - be life threatening! http//www.youtube.com/
watch?vviK121c8iZI
- NO diffuses from endothelium to VSM, activates
guanylate cyclase to produce cGMP. - cGMP, which reduces intracellular Ca by
inactivating an L-type Ca channels. cGMP also
sensitizes the myosin sensitivity to Ca.
9
Smooth muscle integration of vasomotor signals
Note many of these stimuli can cause relaxation
() or contraction depending on location and dose
10
Intrinsic regulation of blood flow
Three kinds of intrinsic regulatory
mechanisms Reactive hyperemia Autoregulation Fu
nctional hyperemia
Reactive hyperemia
11
Intrinsic regulation of blood flow
Three kinds of intrinsic regulatory
mechanisms Reactive hyperemia Autoregulation Fu
nctional hyperemia
Autoregulation
Repays a flow debt incured during a time of
reduced perfusion
12
Intrinsic regulation of blood flow
Three kinds of intrinsic regulatory
mechanisms Reactive hyperemia Autoregulation Fu
nctional hyperemia
Flow rises to supply the necessary O2 for work
13
MECHANISMS INVOLVED IN THE INTRINSIC REGULATORY
PROCESSES
- MYOGENIC MECHANISM
- An inherent property of vascular smooth muscle.
- Stretch leads to contraction
- Probably most important in autoregulation and
reactive hyperemia. - METABOLIC MECHANISM
- Originating from an alteration in the balance
between the metabolic demands of the tissue and
the blood flow and O2 supply. - Increased metabolism leads to dilation via the
release of dilators like adenosine - TISSUE PRESSURE
- Tissue pressure rises with more filtration and
this reduces the filtration pressure back toward
control values. - It may be important in pathological states e.g.
compartment syndrome - Injury may increase vessel permeability
sufficiently to cause major accumulation of fluid
in tissue and vascular occlusion.
14
Myogenic vs metabolic regulation
- Myogenic and the metabolic mechanisms are the
most frequently activated. - varies in different organs under different
conditions. - The strength of one or the other of the
regulatory mechanisms varies in different organs
under different conditions. - Heart relies heavily on metabolic mechanism and
kidney relies heavily on myogenic mechanism - The importance of the metabolic mechanism is
heavily influenced by the normal ratio of flow
(F) to metabolic rate (MR) for a given tissue.
15
CENTRAL REGULATORY RESPONSES OF THE HEART AND THE
VASCULATURE
Receptors
Effectors
chemoreceptors
baroreceptors
atrial receptors
16
BLOOD PRESSURE SENSORS ARTERIAL
Baroreceptors respond to stretch Nerve impulses
over the vagus and glossopharyngeal to medulla
inhibit sympathetic nerve discharge and increase
parasympathetic.
Vasodilation due to reduced contraction of
arterioles. Decrease sympathetic activity also
decreases heart rate and contractility Parasympath
etic decreases rate.
17
The baroreceptors are sensitive to both mean and
pulse pressure.
Experimentally change mean pressure and leave
pulse pressure the same. Note that the
baroreceptor nerve has a greater response to the
pulse pressure as the mean pressure is raised.
Recordings from the glossopharyngeal nerve
18
BLOOD PRESSURE SENSORS - LOW PRESSURE SIDE
- Located in the atria, ventricles, and pulmonary
artery - Two types of atrial receptors
- Atrial A receptors - stimulated by atrial
contraction - Atrial B - stimulated by atrial distention
- Stimulation by stretch causes vasodilation
- These are especially important in blood volume
control - Stimulation also inhibits release of angiotensin,
aldosterone, and vasopressin, all critical
regulators of blood volume.
19
Other receptors regulating CV function
- ENTERIC SENSORS - intestine
- Can produce both vasoconstriction and
vasodilation - Gut distortion or pulling causes a major fall in
resistance. - CUTANEOUS RECEPTORS
- Superficial receptors produce vasoconstriction
- Deep receptors cause vasodilation
20
EXTRINSIC REGULATORY RESPONSES III - EFFERENT
NEURAL PATHWAYS- SYMPATHETIC ADRENERGIC FIBERS
- Transmitter released as a result of nerve
activity is norepinephrine - co-transmitters also released including ATP and
neuropeptide Y (NPY). - This is the dominant means of neural control of
the peripheral circulation. - Norepinephrine is one of a catecholamines and can
stimulate two types of receptors on the blood
vessels - a receptors - contraction of the smooth muscle
- b receptors - relaxation of the smooth muscle
cells - Vessels stimulated with norepinephrine will
normally show only the effects of a stimulation,
because the b stimulating capacity of
norepinephrine is weak. - Epinephrine - more potent b stimulator,
especially at low doses in striated muscle. - low doses - relaxation
- higher doses - constriction.
- Arterioles and venules are both innervated. The
capillaries are not. - Norepinephrine release from sympathetic nerve
terminals causes decreased flow, decreased
capillary pressure, and decreased venous volume.
21
CONTROL OF CAPILLARY FLUID EXCHANGE
Muscle or other tissue on a scale to measure
changes in either blood or interstitial fluid
volume
Initial rapid rise is accumulation of blood in
the tissue, i.e. distension of the vessels. Slow
secondary change has been shown to be due to
fluid filtering from the capillaries into the
space surrounding the tissue cells, the
interstitial space.
22
EFFECT OF SYMPATHETIC STIMULATION ON BLOOD AND
INTERSTITIAL VOLUME
Sympathetic stimulation Constricts the veins
and forces blood out of the tissue and back
to the body Constricts the arterioles,
lowers capillary pressure and causes fluid
reabsorption from the interstitial space
into the blood
23
RELATIVE SENSITIVITY OF RESISTANCE (arterioles)
AND CAPICATANCE (venules) VESSELS
24
TISSUE DIFFERENCES IN RESPONSE TO SYMPATHETIC
STIMULATION
Kidney and intestine are more like skin
25
SYMPATHETIC CHOLINERGIC FIBERS
- The dominant cause of neurally induced
vasodilation is removal of sympathetic tone or
passive dilation. - However, there is a set of fibers that originate
in the motor cortex, and pass through the
hypothalamus where they synapse with fibers from
other areas and then through the medulla and into
the spinal outflow. - Transmitter is acetylcholine and these may induce
an active vasodilation). - These sympathetic cholinergic fibers are not
tonically active and they do not innervate the
capacitance vessels. - Activated by strong emotional influences and the
anticipation of exercise. Function is not well
established. - May be activated during the initial transient
response to baroreceptor stimulation to produce
"active vasodilation."
26
PARASYMPATHETIC DILATOR FIBERS
- Transmitter is acetylcholine
- Fibers of cranial origin supply head and viscera.
- Fibers of sacral origin supply genitalia,
bladder, and large bowel. - In general, activation of these fibers results in
vasodilation of digestive and reproductive
organs. - In the salivary glands, activation of the
parasympathetic nerves produces a unique
collaboration between intrinsic and extrinsic
mechanisms - Bradykinin is one of the most powerful
vasodilators. - In the penis, there is also a non-adrenergic,
non-cholinergic nerve that releases NO which
relaxes the smooth muscle of the arterioles and
of the corpora cavernosum.
27
EXTRINSIC MECHANISMS IV -- HUMORAL PATHWAYS
- ADRENAL MEDULLARY HORMONE
- mainly epinephrine.
- release is stimulated by decrease pressure in the
baroreceptors, emotion, exercise, and a variety
of chemical stimuli. - Activation of the sympathetic nervous system is
manifested primarily by the effects of the nerves
rather than the hormonal epinephrine - Circulating levels of epinephrine at times of
stress are in a concentration range that causes
dilation of the striated muscle vasculature and
constriction of the cutaneous vessels, obviously
ideal in time of danger.
28
EXTRINSIC MECHANISMS IV -- HUMORAL PATHWAYS
- ADRENAL CORTICAL HORMONES
- Corticosterone
- Synthesized and released by the adrenal cortex
- As in the heart a permissive role in maintaining
reactivity to other hormonal and neural
transmitters. - By permissive, one means that the adrenal
cortical hormones have little effect by
themselves, but rather they create conditions in
which the other vasoactive materials are active. - Aldosterone
- Major action is on the kidney
- Increases salt and water retention, and thereby
expands extracellular volume - Tends to elevate blood pressure
29
EXTRINSIC MECHANISMS IV -- HUMORAL PATHWAYS
- ANGIOTENSIN II
- One of the most complex vasoactive substances in
the cardiovascular system - An octapeptide formed from Angiotensin I by
converting enzyme - Formation initiated by low sodium chloride and
low blood pressure in the kidney - Potent vasoconstrictor
- Inhibition of synthesis by angiotensin converting
enzyme (ACE) inhibitors is a common treatment for
hypertension - Highly involved in body salt and water balance
30
EXTRINSIC MECHANISMS IV -- HUMORAL PATHWAYS
- ANTIDIURETIC HORMONE (ADH)
- Also known as vasopressin
- Peptide released by the posterior pituitary
- Potent vasoconstrictor
- Major role is in control of water balance
- important in hemorrhage and also in maintenance
of normal blood pressure - HISTAMINE
- Released by mast cells following injury and
allergic responses - Dilates arterioles, constricts venules
- Increases capillary permeability
31
EXTRINSIC MECHANISMS IV -- HUMORAL PATHWAYS
- PROSTAGLANDINS AND PROSTACYCLINS
- Synthesized from arachidonic acid breakdown
- Synthesized on demand not stored
- Synthesis is blocked by aspirin or other
cyclooxygenase inhibitors - Release is frequently associated with injury
- Many types dilate vessels, constrict vessels,
modify sympathetic nerve transmission
32
Non-steroidal anti-inflammatory drugs
- NSAIDs are generally indicated for the
symptomatic relief of the following conditions! - Rheumatoid arthritis
- Osteoarthritis
- Inflammatory arthropathies (e.g. ankylosing
spondylitis, psoriatic arthritis, Reiter's
syndrome) - Acute gout
- Dysmenorrhoea (menstrual pain)
- Metastatic bone pain
- Headache and migraine
- Postoperative pain
- Mild-to-moderate pain due to inflammation and
tissue injury - Pyrexia (fever)
- Ileus
- Renal colic
33
(No Transcript)
34
Cardiac output determines venous return
determines cardiac output determines venous
return determines venous return determines
cardiac output
35
Troponin I stimulation of an inhibitor
- Troponin C in cooperation with tropomyosin
regulates myocyte contractile force. - Phosphorylation of troponin I by protein kinase A
causes a reduction in the Ca affinity of
troponin C. The resulting desensitization of the
myofilament response to Ca increases the rate
of relaxation.
36
Viagra the long and the short of it
- Relaxation causes inflow of blood and filling of
the vessels to produce erection - decrease of sympathetic vasoconstrictor outflow
to the penis - activation of parasympathetic, non-adrenergic,
non- - cholinergic (NONAC) neruons and release of
nitric oxide - NO, via cGMP and protein phosphorylation
reduces smooth - muscle Ca and desensitizes the contractile
proteins - response to Ca
relaxation of the muscles controlling penile
blood flow and the sinuses of the corpora
caveronosa erection - Effects are reversed by phosphodiesterase
5 - Viagra inhibits the phosphodiesterase and
prolongs the - erection
37
Health Library
HEALTH LIBRARY
Report Viagra may help enlarged hearts Sunday,
January 23, 2005 Posted 451 PM EST (2151 GMT)
Follow the news that matters to you. Create your
own alert to be notified on topics you're
interested in.Or, visit Popular Alerts for
suggestions.