Learning Objectives PowerPoint PPT Presentation
1 / 79
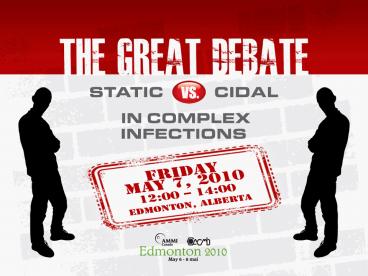
Title: Learning Objectives
1
(No Transcript)
2
Learning Objectives
- Understand the definition of bactericidal and
static therapies - Identify the advantages and limitations of cidal
and static therapies - Assess the significance of evidence related to
cidal versus static therapies and determine their
applicability in those with complex infections
3
- Which of the following regions are you from?
- Atlantic
- Quebec
- Ontario
- BC
- Prairies
- Other
4
- How do you identify yourself primarily
- Adult ID
- Paed ID
- Medical microbiology / clinical microbiology
- Intensivist
- Industry?
5
- How long have you been in practice?
- 0-10 years
- 10-20 years
- 20 years
- None of your business
6
- Which team will get further in the NHL playoffs?
- Canadiens
- Penguins
- Bruins
- Flyers
- Raptors
7
Case Question
- A 58 year old woman presents with fever of 38.6.
- She has had a left arm PICC for the last 2 months
for chemo Rx - for breast cancer. She is alert and normotensive.
She is not - neutropenic and has not had chemo for 5 wks. A
blood culture is - collected and grew MRSA. A TEE is normal.
- You remove the PICC and prescribe which
antibiotic - Single bactericidal agent
- Single bacteriostatic agent
- 2 antibiotics
- Doesnt matter
8
The Case for Bacteriostatic Antibiotics in
Complex Infections
- Edward A. Dominguez, MD FACP FIDSA
- Methodist Transplant Physicians
- Dallas, Texas, USA
9
Disclosures for E A Dominguez
- Pfizer Consultant Speaker bureau Advisory
boards - Cubist Speaker bureau
- Astellas Speaker bureau
10
Whats in Play?
- Bacterial infections
- Definitions and their limitations
- Is an antibiotic cidal, static, or both?
- Disadvantages of bactericidal therapy
- Advantages of bacteriostatic therapy
- A sampling of static vs. cidal studies
11
Whats NOT in play?
- Antifungal therapy
- Antiparasitic therapy
- Antiviral therapy
- Monotherapy vs. combination therapy
12
What is Cidal? What is Static?
- Concept is only 35 years old
- Shah PM, et al. Dtsch Med Wochenschr.
1976101325-328. - Two components to the distinction
- MBC/MIC
- Static MBC/MIC 16
- Cidal MBC/MIC 4
- Time-Kill curve
- Cidal if gt 3-log reduction in CFU/ml after 24
hours incubation in liquid media (standard
inoculum 5 x 105 CFU/ml in a volume of 0.01 ml)
13
The Tool Time-Kill Curve
- Provides full dynamic profile of antibiotic
- Determines concentration response relationships
- Provides insight into potential for resistance
development and for drug synergy - Provides log-linear killing rate and cidal rate
constant
14
Problems with the Time Kill Curve
- Growth conditions (e.g. pH, protein binding)
- Test duration (18-24 hrs)
- Testing done in log-phase growth, but most
bacteria causing infections are in stationary
phase1,2 - Unclear if there is clinical utility3
- Strictly interpreted, interpretation only applies
to the tested organism under tested conditions
- Kim KS, et al. Antimicrob Agents Chemother.
1981191075-77. - Eng RH, et al. Antimicrob Agents Chemother.
1991351824-28. - Peterson LR, et al. Antimicrob Agents Chemother.
197813665-68.
15
Which Side is Your Antibiotic On?
- Bacteriostatic
- Macrolides
- Tetracyclines
- Glycylcyclines
- Sulfonamides
- Clindamycin
- Linezolid
- Bactericidal
- ?-lactams
- Aminoglycosides
- Vancomycin
- Flouroquinolones
- Daptomycin
- Metronidazole
16
However Some are Both4
- Macrolides may show in vitro bactericidal
activity vs. S. pneumoniae and S. pyogenes. - Linezolid shows in vitro bactericidal activity
vs. S. pneumoniae and other streptococci. - Quinupristin-dalfopristin shows in vitro
bacteriostatic activity vs. E. faecium.
4. Pankey GA, Sabath LD. Clinical Infect Dis.
2004381864-70.
17
The Problem of Inoculum
- MBC testing standard uses concentration of
bacteria of 105 in log-phase. - Many localized infections have bacterial
concentrations of 108-10 CFU/gm tissue, mostly in
stationary phase.5 - These conditions may render cidal antibiotics
ineffective - Vancomycin for experimental GPC endocarditis6
- Penicillin for experimental S. pyogenes thigh
abscesses7
- Levison ME, et al. Infect Dis Clin North Am.
19893415-421. - Cantoni L, et al. Antimicrob Agents Chemother.
1990342348-53. - Stevens DL, et al. J Infect Dis. 198815823-8.
18
Disadvantages of Bactericidal Therapy
- Rapid lytic action may lead to endotoxin surge
- Gram-negative meningitis in infants11
- Infant botulism12
- Enterohemorrhagic E. coli infection13
- Increased cerebral edema
- Pneumococcal meningitis14
- Mustafa MM, et al. J Infect Dis. 1989160891-95
- Johnson RO, et al. Am J Dis Child.
1979133586-93. - Nau R, et al. Clin Microbiol Rev. 20021595-110.
- Friedland IR, et al. Lancet. 1992339405-08.
19
Advantages of Bacteriostatic Therapy
- THE major advantage may be in some
toxin-producing bacterial infections - Clindamycin inhibits TSST-1 by S. aureus
regardless of growth phase8 - Clindamycin is more effective than penicillin in
models of S. pyogenes and C. perfringens
myositis9-10 - Long post-antibiotic effect
- Efficacy correlates usually with 24-hr AUC/MIC
- Van Langevelde P, e al. Antimicrob Agenst
Chemother. 1997411682-85. - Stevens DL, et al. J Infect Dis. 1987155220-28.
- Stevens DL, et al. J Infect Dis. 198815823-28.
20
Tygecycline Community Acquired Pneumonia Studies15
15. Tanaseanu, et al. Diagn Microbiol Infect Dis.
200861329-38.
21
Tygecycline CAP Studies Pneumococcal Bacteremic
Patients
22
Linezolid Nosocomial Pneumonia Studies16
Intent-to-treat analysis of prospective studies
16. Wunderink RJ, et al. Chest. 20031241789-97.
23
Speaking of Linezolid
- Linezolid is bacteriostatic vs. S. aureus
- Rabbit S. aureus endocarditis model17
- Bacteriostatic when using standard intermittent
infusion - Bactericidal when using continuous infusion to
maintain levels gt MIC
17. Jacqueline C, et al. Antimicrob Agents
Chemother. 2002463706-11.
24
Conclusions
- In vitro definition may not correlate with in
vivo activity - Clinical distinction between bacteriostatic and
bactericidal activity is situational - Site of infection
- Inoculum of bacterial
- PK/PD characteristics of the antibiotic
- Host defense mechanisms
- For many infections, there is no proven
superiority for bactericidal therapy
25
(No Transcript)
26
Cidal vs Static AntibioticsThe Pro-Cidal
pointor The worse the disease, the more cidal
agent is preferred
- Ethan Rubinstein MD, LL.b.
- University of Manitoba
27
Conflicts
- Consultant Astellas, Aventis-Sanofi, Atox,
Bayer, BiondVax, MeMed, Cubist, Fab Pharma, J
J, Pfizer, Merck, Theravance, Wyeth Canada, - Research grants Daiichi, Bayer, Theravance,
AstraZeneca - Speakers Bureau Merck-Canada, Astellas-Canada,
Pfizer Int. Pfizer-Canada, Aventis-Sanofi
28
Why do we care if an anti-microbial agent is
bactericidal?
- What is a bactericidal agent?
- What are the rules for determining whether a drug
is static or cidal? - Under what clinical situations is a cidal agent
mandated? Preferred? - Under what clinical situations might the use of a
cidal agent be bad? Why?
29
Question 1 Under which clinical situation(s)
would a rapidly bactericidal agent be bad?
- Endocarditis
- Pneumococcal bacteremia
- Osteomyelitis
- Leptospirosis
- Brain abscess
30
Answer
- 4. Leptospirosis/ Tertiary syphilis
- Reason Jarish Herxheimer Reaction in Syphilis,
Lyme, leptospirosis-rapid release of toxins
causing fever hypotension leucocytosis etc.
31
(No Transcript)
32
Tops Textbook of Infectious Diseases, 1960
- WHILE IT IS TRUE THAT MANY DRUGS ARE
BACTERIOSTATIC AT A MUCH LOWER CONCENTRATION THAN
THAT AT WHICH THEY ARE BACTERICIDAL, ALMOST ALL
AGENTS ARE ULTIMATELY FATAL IF A SUFFICIENT LEVEL
IS REACHED . The best definition is generally
obtained with - the concentration which is usually found in
serum. It has been very difficult to establish
the importance of killing power as a factor in
clinical results because it is only one of
several factors
33
Question 2 How is bactericidal activity defined?
- Animal studies
- In vitro studies
- Clinical trials
- Combination of the above
34
Answer to question 2
- 2. In vitro studies only
35
What is a bactericidal agent?
Bactericidal kill of 99.9 of bacteria in vitro
within 18-24 h. Bacteriostatic kill of 90-99
of bacerial inoculum within 18-24 h
36
Definition of Bactericidal
37
Method of Defining Bactericidal Activity
- Figure. A fixed culture of bacteria is added to
each of the 6 test tubes. - The first tube serves as the growth control, and
no antibiotic is added to this tube. - Tubes 26 contain antibiotic in serially diluted
proportions ranging from 0.5 to 8 mg/mL. - After 1824 h of incubation, the first tube that
appears visibly clear represents the MIC. - However, to determine the minimum bactericidal
concentration (MBC), each tube is subsequently
plated onto agar plates and incubated. The first
serial plated agar dish demonstrating no growth
(or a 99.9 decrease) represents the MBC. In the
case above, the MIC is 2 µg/mL, and the MBC is 4
µg/mL
Critical issues Inoculum gt 5 x105 cfu/mL
Sub-culture volume 0.1 mL to
predict gt99.9 kill
Static MBC MIC ratio gt 4
NCCLS Document M26-A, 1999
38
Problems with the in vitro testing
- Static antibiotic concentration- while in the
body concentration fluctuates - Fixed number of bacteria (never in the body)
- Logarithmic growing bacteria (in the body
bacteria are in log stationary phases) - Lack of serum (protein binding)
- Transfer of antibiotic during sub-culturing
- Utility of SBT is not clinically proven
39
(No Transcript)
40
(No Transcript)
41
Cidal vs Static antimicrobial agents
- Drugs that bind to the cell wall like penicillin
are likely to be cidal whereas agents that
interfere with metabolic pathways like
sulfonamide drugs and folate antagonists are
likely to be static, exceptions exist - An antimicrobial agent can be cidal for one
strain and static for another strain of the same
organism
42
Antimicrobial properties of chemotherapeutic
agents
43
Is a cidal agent always better?
44
(No Transcript)
45
Shortcomings of cidality
- The Eagle Musselman paradoxical effect
- Tolerance is when MBC is 32 times the MIC
46
Question 3 In which clinical condition have
bactericidal agents shown to be superior to
static agents?
- Streptococcal throat
- Urinary tract infection
- Bacterial meningitis
- Septic shock
- Typhoid fever
47
Answer
- 3. Bacterial meningitis
48
Based on which data?
- Historical Data Pneumococcal meningitis
- Treatment of bacterial endocarditis
- Animal models
49
Question 4 In a patient highly allergic to
penicillin that presents with lobar pneumonia and
bacteremia caused by S. pneumoniae which
agent would you prefer?
- Sulfa-agent
- Low dose Chloramphenicol
- Low dose Quinupristin/Dalfopristin
- Low dose Linezolid
- High dose Linezolid
50
Answer to question 3
- 5. High dose Linezolid
- Bostic et al. Diagnost Microbiol Infect Dis
199830109-112 - Zuenko et al. Antimicrob Agents Chemother 1996
40839 - Pankey Sabath Clin Infec Dis 200438864
51
Historical Experience with Treatment of
Endocarditis
- Prior to the advent of penicillin, endocarditis
was uniformly fatal despite the success of sulfa
drugs for streptococcus - The use of high dose penicillin led to cures of
streptococcal endocarditis - The use of penicillin for enterococcal
endocarditis did not improve mortality - The addition of aminoglycosides to penicilllin
resulted in cures of enterococcal endocarditis - This correlated with the bactericidal activity of
the antimicrobial agents
52
(No Transcript)
53
Treatment of Meningitis
- The Lepper and Dowling study
- Treatment of Pneumococcal Meningitis
- Mortality- Penicillin alone 21
- Mortality- Penicillin plus chlortetracycline
(Aureomycin) 79 - Lepper MH, Dowling HF. Treatment of pneumococcal
meningitis with penicillin compared with
penicillin plus aureomycin. Arch Intern Med
195188489.
54
Treatment of Meningitis The Mathies Study
- Treatment of children with meningitis
- Ampicillin alone- mortality 4.3
- Ampicillin, chloramphenicol, and streptomycin-
mortality 10.5 - Mathies AW Jr, Leedom JM, Ivler D, Wehrle PF,
Portnoy B. Antibiotic antagonism in bacterial
meningitis. Antimicrobial Agents Chemother
19677218-224.
55
Issues with these studies
- They are small
- They are not randomized
- They do not look carefully at the microbes
involved - Why is this important?
56
How do you know if an anti-microbial agent is
Cidal or Static?
- The case of chloramphenicol
- Chloramphenicol was used for many years as the
drug of first choice for meningitis. - Is chloramphenicol a cidal or static agent?
- It is cidal against H. influenzae and S.
pneumoniae and is an effective treatment for HiB
S. pneumo meningitis it is static against
enterobacteriaceae and should not be used in
Gram(-) meningitis
57
Listeria meningitis
- Common cause of meningitis in immunocompromised
patients - Ampicillin is bacteriostatic for most strains
- Vancomycin, aminoglycosides, and tmp/sulfa have
bactericidal activity against most strains - Hof H, Nichterlein T, and Kretschmar M. Clinical
Microbiology Reviews 199710345-357.
58
How should we treat Listeria meningitis?
59
Listeria meningitis
- Most authorities recommend Ampicillin (with or
without aminoglycosides) as the drug of first
choice for Listeria meningitis - Studies in humans do not provide clear evidence
for the superiority of any regimen - One study of 22 patients suggests a combination
of Ampicillin-cotrimoxazole may be superior to
Ampicillin-aminoglycoside - Merle-Melet, M. Dossou-Gbete, L. Maurer, P. et al
Journal of Infection 19963379-85.
60
One study of 22 patients suggests a combination
of Ampicillin-cotrimoxazole may be superior to
Ampicillin-aminoglycoside Merle-Melet, M.
Dossou-Gbete, L. Maurer, P. et al Journal of
Infection 19963379-85.
61
Does one always want to use a cidal antibiotic?
62
Urinary Tract Infections
- Treatment of E. coli UTIs
- Which is cidal- Ampicillin or TMP/Sulfa?
- Which would you chose?
- A series of studies of treatments of
uncomplicated UTIs in the 1970s indicated
superiority of TMP/Sulfa vs Ampicillin - Many authorities now use fluoroquinolones but
this is related to local susceptibility issues
63
When is a Cidal Agent bad?
- Rabbit model three hours after treatment of E.
coli meningitis with cefotaxime, increased
endotoxin was found in the CSF of rabbits. - No endotoxin was seen in rabbits treated with
chloramphenicol - Brain edema was less in the chloramphenicol
treated rabbits - Friedland IR, Jafari H, Ehrett S, et al. J Infect
Dis 1993168657-662.
64
- While cefotaxime, a cidal agent, reduced
bacterial titers faster, more endotoxin was
produced in early time points - After 6 hours however, there was more LPS in the
chloramphenicol treated animals and the bacterial
titers were higher - A series of animal studies suggest a role for
rifampin in experimental meningitis - Nau R and Eiffert H. FEMS Immunology and Medical
Microbiology 2005 441-16.
65
Treatment of Meningitis
- Current clinical practice in treatment of
meningitis in humans - Is to use steroids as modulators of inflammation
- In general success or failure may be more likely
to be related to the ability to rapidly sterilize
the CSF than to whether the agents employed are
static or cidal
66
Clinical Situations where cidal agents are
preferable
- Endocarditis
- CNS infections
- Infections in immunocompromised patients
- Osteomyelitis?
67
Question 5
- In general Severe diseases need cidal agents
- true
- false
68
Under what other clinical situations might the
use of a cidal agent be bad? Why?
69
What might a cidal agent be bad?
- Toxin production by microbes may induce host
responses S. aureus sepsis - In a mouse model, the use of clindamycin may lead
to less release of proinflammatory cytokines
than ceftriaxone - Mortality and morbidity was decreased in the
clindamycin treated group - Azeh I, Gerber J, Wellmer A et al, Crit Care Med
2002301560-1564.
70
SUMMARYWhen might a cidal agent be bad?
- When a disease is associated with the release of
a toxin (e.g. Staphylococcal toxins or E. coli
enterotoxins) - Antimicrobials that diminish toxin release might
be beneficial - On the other had if the microbes continue to
divide, the advantage may be offset by the
failure to eliminate the pathogen
71
When does it matter?
- Studies of endocarditis indicate that
bactericidal agents are more effective than
static drugs (penicillin vs erythromycin)
72
OVERALL CONCLUSIONS-1
- In the treatment of bacterial endocarditis,
bactericidal antibiotics are preferred - In the treatment of CNS infections, rapid
sterilization of the CSF may be more important - In some areas (prevention of Staph. aureus wound
infections), whether an antibiotic is static or
cidal does not appear to matter
73
OVERALL CONCLUSIONS
- In clinical practice, issues such as
susceptibility of the organism, penetration of
the antimicrobial agent and rapid inhibition of
replication of microbe are likely to be critical
to the success of therapy
74
(No Transcript)
75
Static- Cidal in 2010 does it really
matter? The greater the ignorance the greater
the dogmatism
76
See you when you have convincing new data
77
REBUTTAL
78
Addressing the Classical Bactericidal Conditions
- Endocarditis
- Osteomyelitis
- Meningitis
- Neutropenic fever
79
Bacterial Endocarditis
- High density (1010) of non-replicating bacteria1
- Staphylococcal endocarditis
- Clindamycin had 70 cure rate in early study2
- Similar cure rates using ß-lactam
aminoglycosides3-4 - Vancomycin-resistant enterococcal (VRE)
endocarditis - Oral linezolid has cured select cases5-6
- Anectdotal only NOT approved for this indication
- Durack DT, et al. Br J Exp Pathol. 19725344-9.
- Watanakunakorn C. Am J Med. 197660419-25.
- Musher D, et al. Medicine (Baltimore).
197756383-409. - Korzeniowski O, Sande M. Ann Intern Med.
198297496-503. - Babcock HM, et al. Clin Infect Dis.
2001321373-75. - Moise PA, et al. J Antimicrob Chemother.
2002501017-26.
80
Bacterial Osteomyelitis
- Bone concentrations of many drugs is poor
- BUT, tetracyclines and clindamycin achieve high
concentrations - Extensive favorable experience with clindamycin
for gram-positive osteomyelitis7 - Antibiotics may be adjunctive therapy to surgery
for some (e.g. diabetic foot infection)
- Mader J, et al. Clin Orthop. 199329587-95.
81
Bacterial Meningitis
- In CSF, there is reduced neutrophil phagocytic
activity - Bacteriostatic agents with good CSF penetration
- Tetracyclines
- Chloramphenicol
- Linezolid
- Trimethoprim-sulfamethoxazole (TMP-SMX)
82
Bacterial Meningitis
- Tetracycline terramycin effective in early trial8
- Chloramphenicol variably effective9
- NOT for pcn-resistant pneumococcal disease
- Linezolid effective in some cases of VRE
meningitis10 - TMP-SMX used in bacterial meningitis11 and
ventriculoperitoneal shunt infections12
- Hoyne AL, Simon DL. Arch Pediatr. 195370319-25.
- Paredes A. Pediatrics. 197658378-81.
- Zeana C, et al. Clin Infect Dis. 200133477-82.
- Levitz RE, et al. Ann Intern Med.
1984100881-90. - Dominguez EA, et al. Clin Infect Dis.
199419223-24,
83
Neutropenic Fever
- I have no reliable data to refute the perceived
benefit of bactericidal monotherapy or
combination therapy in this disease.
84
Is This Distinction Outdated?
- Another antibiotic mechanism for transcription or
translation inhibitors13 - Triggering bacterial toxin-antitoxin chromosomal
modules (e.g. mazEF) - Leads to cell death via Reactive Oxygen Species
- Quorum-sensing communication factors may mediate
bacterial apoptosis (in dense culture)14 - Extracellular Death Factor (EDF), when added to
E. coli, modulates mazEF - Induces rifampacin to become bactericidal rather
than bacteriostatic15
- Engelberg-Kulka, et al. Communicative Integrative
Biol. 20092211-12. - Kolodkin-Gal I, et al. Science. 2007318652-55.
- Kolodkin-Gal I, et al. PLoS Biology. 20086319.
85
Conclusions
- In vitro definition may not correlate with in
vivo activity - Clinical distinction between bacteriostatic and
bactericidal activity is situational - Site of infection
- Inoculum of bacterial
- PK/PD characteristics of the antibiotic
- Host defense mechanisms
- For many infections, there is no proven
superiority for bactericidal therapy
86
Merci Beaucoup!
87
Rebuttal
88
If static are good and cidal are good (or better)
shouldnt the combination work?
Lepper Dowling Arch Int Med 1951
89
Frequency of Death and Severe neurological
residua(Mathies et al. A A C 19677218)
90
Time for Death in Combi. Rx
(Mathies et al. A A C 19677218)
91
- Which team will get further in the NHL playoffs?
- Canadiens
- Penguins
- Bruins
- Flyers
- Raptors
92
Case Question
- A 58 year old woman presents with fever of 38.6.
- She has had a left arm PICC for the last 2 months
for chemo Rx - for breast cancer. She is alert and normotensive.
She is not - neutropenic and has not had chemo for 5 wks. A
blood culture is - collected and grew MRSA. A TEE is normal.
- You remove the PICC and prescribe which
antibiotic - Single bactericidal
- Single bacteriostatic effect
- 2 antibiotics
- Doesnt matter
93
Housekeeping
- Evaluations
- Certificate of Attendance