Age related cognitive decline PowerPoint PPT Presentation
1 / 37
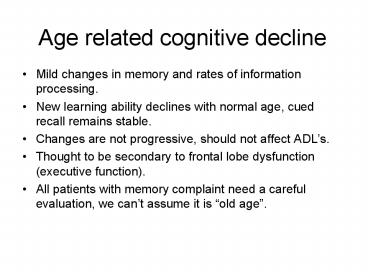
Title: Age related cognitive decline
1
Age related cognitive decline
- Mild changes in memory and rates of information
processing. - New learning ability declines with normal age,
cued recall remains stable. - Changes are not progressive, should not affect
ADLs. - Thought to be secondary to frontal lobe
dysfunction (executive function). - All patients with memory complaint need a careful
evaluation, we cant assume it is old age.
2
Mild Cognitive Impairment
- Phase between normal aging and dementia.
- Cognitive impairment is documented but not severe
enough to interfere with ADLs. - May represent a pre-demented state.
- Increased risk for progressing to AD (12 per
year vs 1-2 for matched controls). - Studies under way to determine if current (AD)
treatments can slow this rate of progression. - Guidelines from AAN recommend monitoring this
patients closely.
3
Dementia
- Progressive decline in multiple cognitive and
behavioral domains - memory
- language and speech
- visuospatial ability
- abstract thinking
- judgment
- mood and personality.
- Changes are severe enough to interfere with
social and occupational functioning (ADLs). - Changes do not occur exclusively during delirium.
4
Dementia Differential Diagnosis
- Cortico-degenerative
- Alzheimers disease
- Frontotemporal dementia
- Vascular
- Multiple large vessel infarcts
- Single strategic infarct
- Lacunar state
- Binswangers disease
- CADASIL
- Parkinsonism-related demetias
- Parkinsons disease
- Dementia with Lewy Bodies
- Progressive supranuclear palsy
- Multiple systems atrophy
- Dementias associated with infection
- Prion diseases
- Neurosyphilis
- AIDS dementia
- Chronic meningitis(TB, fungal)
- Toxic-Metabolic conditions
- Medication-induced dementia
- Alcohol related dementia
- Heavy metal exposure
- Vitamin B12, folate deficiency
- Cushings, Addisons disease
- Hypo-hyperthyroidism
- Liver, renal failure
- Paraneoplastic (Limbic encephalitis)
- Autoimmune/Inflamatory
- Bechets disease
- Multiple sclerosis
- SLE, Sarcoid
- Temporal arteritis/other CNS vasculitis
- Trauma-related dementias
- Closed-head injury
- Chronic SDH
- Dementia pugilistica
- Miscellaneous
5
Alzheimers Disease
Dementia Differential Diagnosis
- Onset is insidious and progression slow (average
decline 8-10 yrs). - Features include
- Language disturbances (early) anomia/fluent
aphasia/paraphasias/impaired comprehension - Recent memory/learning impairment
- Apraxia/constructional ability
- Agnosia
- Alexia
- Behavioral disturbances (may precede cognitive
impairment) - Delusions/hallucinations in 50
- Lack of insight
6
Vascular Dementia
Dementia Differential Diagnosis
- Vascular lesions contribute to development of
dementia. - Second most common cause of dementia after AD
(10-20). - Diagnosis suggested if
- Onset of cognitive deficits associated with
stroke - Abrupt onset of symptoms with stepwise
deterioration - Neurologic exam c/w prior stroke
- Infarcts on cerebral imaging
- Presentation varies depending on location of
infarcts.
7
Vascular Dementia and AD
Dementia Differential Diagnosis
- Vascular pathology exists in 29-40 of dementia
patients coming to autopsy. - Adjuvant role of vascular lesions in AD.
- CVD determines presence and severity of AD
symptoms - Study of 61 patients with pathologic AD criteria
- Those with brain infarcts had poorer cognitive
function and higher incidence of dementia - A relative small number of AD lesions resulted in
dementia in those with lacunar infarcts. - Diagnosis of AD plus CVD determined by imaging
and clinical course.
8
Frontotemporal dementias
Dementia Differential Diagnosis
- Heterogeneous group of disorders 2ry to
degeneration of frontal lobes. - Includes Picks disease.
- Prominent behavioral changes (early)
- Disinhibition, impulsiveness, apathy, social
inappropriateness. - Language disturbances
- Reduction of speech, echolalia, perseveration
- Deficits in social comportment, behavior,
language are out of proportion to memory deficit. - Neuroimaging visualizes frontal lobe atrophy.
- SPECT fronto-temporal lobe hypoperfusion
(earliest sign).
9
Parkinsonism related dementias
Dementia Differential Diagnosis
- Parkinsons disease dementia
- Complicates PK in 40, cognitive decline 1 year
after movement disorder. - Impaired recall, executive function.
- Language intact.
- Dementia with Lewy bodies
- Fluctuating cognitive performance
- Prominent visual hallucinations
- Cognitive impairment and parkinsonism emerge
simultaneously - Severe adverse reaction to neuroleptics used for
behavioral problems. - Progressive supranuclear palsy
- Multisystem atrophy
- Vascular parkinsonism
- Cortico-basal ganglionic degeneration
10
Reversible dementias
Dementia Differential Diagnosis
- Depression
- Medication induced (analgesics, anticholinergics,
psychotropics, sedatives). - Alcohol related (intoxication, withdrawal)
- Metabolic disorders
- Thyroid disease
- B12 deficiency
- HypoNa, hyperCa
- Liver and renal dysfunction
- Infectious
- AIDS, syphilis, chronic meningitis.
- C-J disease Rare, rapidly progressive,
incurable, dementia. - Cognitive impairment, motor deficits, seizures
- SDH, CNS neoplasms
- NPH triad of gait disturbance, incontinence and
cognitive dysfunction
11
Depression
Reversible dementias
- Common cause of reversible dementia in elderly.
- Complex relationship between depression and
cognitive impairment - Elderly depressed patients are a higher risk of
developing dementia. - Demented patients can show apathy, sleep problems
resembling depression. - depressive pseudodementia
- Both have very poor insight on mood and
cognition. - No reliable tool to measure relative contribution
of each. - Screen for depression and treat if present.
- Follow patients and assess for improvement.
12
Delirium
Reversible dementias
- Acute confusional state associated with systemic
illnesses, infections, toxic and metabolic
disturbances. - Characterized by
- Disturbance of consciousness
- Change in cognition
- Rapid onset and fluctuation of symptoms
- Patients with dementia are at increased risk for
delirium. - Delirium and dementia may coexist.
13
Dementia Diagnostic approach
- Not all patients with complaints of memory loss
have dementia. - Step 1 determine if true cognitive impairment is
present. - Step 2 think of other conditions that can lead
to memory or cognitive impairment. - Step 3 determine the nature of the dementing
disorder.
14
Step 1 Is there cognitive impairment?
- A full dementia evaluation cant be completed in
40 min. - The initial visit should focus on
- History
- Physical Exam
- Medications
- Labs if indicated
- At follow-up visit arrange time for
- Mental status examination/assessment of cognitive
function - Full neurologic exam
- Review labs
- Imaging studies if indicated.
15
Step 1 Is there cognitive impairment?
- I. History
- History should be obtained from patient and
family. - Self reported memory loss doesnt appear to
correlate well with future development of
dementia. - Informant-reported memory loss is a much better
predictor of the current presence or future
development of dementia. - Focus history on
- Cognitive impairment
- Behavioral disturbances
- Functional impairment
16
Step 1 Is there cognitive impairment?
- Cognitive impairment
- time, character, pattern of progression.
- Life events temporally related to onset.
- Ability to learn and recall new information.
- Informant Questionnaire on Cognitive Decline in
the Elderly. - Behavioral disturbances
- Often the cause to seek medical attention.
- Memory impairment is not always the presenting
feature. - Delusions, hallucinations, changes in mood.
- Changes in personality (disinhibition,
impulsivity, anger, agitation, anxiety). - Functional impairment
- Assess the impact on patients social and basic
functioning. - Some knowledge of patients previous activities
is necessary. - Standarized instruments can be used (Instrumental
ADL Scale).
17
Step 1 Is there cognitive impairment?
- II. Medications
- III. Family and Social Hx
- IV. Physical Examination
- Neurologic exam
- Focal neurologic deficits
- Signs of parkinsonism cogwheel rigidity, tremor
- Gait
- Eye movement
18
Step 1 Is there cognitive impairment?
- V. Mental Status Examination
- Level of consciousness, orientation, attention,
speech and language, recent end remote memory,
cognition, visuospatial skills, mood/personality. - Standarized instruments (MMSE, ADAS, clock
drawing, etc). - Variable sensitivity/specificity depending on
population. - Affected by education and culture.
- Useful in dementia diagnosis when used along
history and exam. - Scores are useful to measuring change over time.
19
Mini Mental Status Examination
- Most commonly used cognitive screening instrument
in US clinical practice. - Maximal score is 30 points.
- Score lt24 suggests dementia (sens 87/spec 82).
- Age-specific norms that incorporate gender and
level of education have been established. - Not sensitive for diagnosis of mild dementia.
20
Step 1 Is there cognitive impairment?
21
Step 1 Is there cognitive impairment?
- VI. Neuropsychologic testing
- Helpful in age-related vs MCI vs dementia.
- Useful for those gray area patients
- MMSE scores 20-25.
- Functional impairment out of proportion to MMSE
scores. - Poor MMSE scores with little functional
impairment. - R/o pseudodementia
- Assists in narrowing differential diagnosis of
dementia syndrome.
22
Step 2Problems presenting as memory loss
- Normal aging
- MCI
- Depression
- Delirium
- Stroke Syndromes
- Bradykinesia
- Abulia
- Seizures
- Excessive daytime somnolence
- Amnestic syndrome
23
Step 3 What is the nature of the dementing
disorder?
- Alzheimers disease 60-80
- Vascular multi-infarct dementia 10-20
- Parkinsons disease and related dementias 5
- Frontotemporal degeneration
- Potentially reversible causes
- Medication induced
- Alcohol related
- Metabolic disorders
- Depression
- NPH
- Remember Dementia frequently has multiple causes.
24
Step 3 What is the nature of the dementing
disorder?
- Laboratory testing
- CBC
- Electrolytes
- B12, folate
- TSH
- BUN/Cr
- LFTs
- RPR not indicated unless clinical suspicion.
- HIV, ESR, toxins, heavy metals, drugs if
indicated.
25
Step 3 What is the nature of the dementing
disorder?
- Laboratory testing
- LP lt55yo, rapid progression, immunosuppr.,
unusual dementia - High CSF protein 14-3-3 96sens/99spec for C-J
disease. - High CSF tau and low ßAmyloid1-42 proteins.
- EEG distinguishes dementia from other diseases..
- Genetic testing for ApoE4 useful in patients
with gt3 first-degree relatives w/demetia.
26
Step 3 What is the nature of the dementing
disorder?
- Neuroimaging
- Obtain CT or MRI in all patients.
- Important to r/o structural lesions SDH, tumor,
NPH. - Essential for diagnosis of VaD.
- MRI
- more sensitive for small CVD lesions as well as
early AD changes. - Important in documenting clinically silent
lacunar infarcts, IWMC, cortical infarcts and
atrophy. - Structural MRI future use in early AD diagnosis.
- SPECT, PET scan not recommended in routine
evaluation.
27
Dementia Treatment
- Rapidly evolving field.
- Better and new understanding of dementing
illnesses. - Management is changing from symptomatic to
biologically specific. - New disease-specific, disease-modifying
treatments are close to being used. - Accurate diagnosis of type of dementia is
essential. - Treating patient with dementia should also
include - Addressing safety issues
- Addressing caregiver needs and concerns
- Screening and treating for depression
- Management of other medical problems
28
Dementia Treatment
- Safety Issues
- Driving
- Cooking
- Wandering
- Aggressive Behavior
- Falls
- Falls are a problem in all dementias
- Study 1608 pts gt75yo showed twice risk of hip fx
if MMSE score was 18-23 compared to pts with
normal scores. - Always evaluates pt that fall B12, myelopathy
(C-spine spondylosis), neuropathy, visual
impairment.
29
Dementia Pharmacologic treatment
- Symptomatic treatment of memory impairment
- Cholinesterase inhibitors
- NMDA receptor antagonists
- Symptomatic treatment of behavioral disturbances
- Delusions and halluciantions
- Depression
- Aggression and anxiety
- Disease modifying treatments
- Vitamin E and selegiline
- Estrogen replacement
- NSAIDS
- Ginkgo biloba
- Secretase inhibitors
- Immunotherapy
30
Pharmacologic treatment of dementiaCholinesteras
e inhibitors
- Patients with AD have impaired cortical
cholinergic function. - Cholinesterase inhibitors can improve cognitive
function in patients with AD. - Average benefit is small, significant in long
term outcomes (NHP). - Meta-analysis 29 RCT improvement of 0.1 SDs on
ADLs, 0.09 SDs on IADLs - Four FDA approved drugs
- Tacrine
- Donepezil
- Rivastigmine
- Galantamine
31
Cholinesterase inhibitors
- Donepezil (Aricept)
- Little peripheral activity, well tolerated.
- Once daily dosing, start 5mg qd for 4 weeks, then
increase to 10mg qd. - 24-week double blind study of patients with
mild-mod AD - 5-10mg vs placebo showed significant improvement
(ADAS-cog) - No consistent effect on QL measures, no effect on
underlying disease course. - 20 SE (nausea, diarrhea, vomiting).
- Prolonged treatment safe.
- May be useful for patients with PD and dementia.
32
Cholinesterase inhibitors
- Rivastigmine (Exelon)
- Beneficial in patients with mild-moderate AD.
- Efficacy comparable to donezepil, more GI side
effects. - Start 1.5mg BID and titrate every two weeks to
6mg BID with meals. - Galantamine (Reminyl)
- Efficacy comparable to donezepil in mild-moderate
AD. - 2 RCT showed 24-32mg/day slowed decline in
cognition and ADLs. - Similar, modest benefits in patients with VaD or
AD plus CVD.
33
Pharmacologic treatment of dementiaNMDA
receptor antagonists
- Glutamate principal excitatory neurotransmitter
in cortical and hipoccampal neurons. - NMDA (N-methyl-D-aspartate) receptors are
involved in memory and learning. - Ischemia induces excessive NMDA stimulation
glutamate-induce excitotoxicity. - NMDA receptor antagonists (memantine) may protect
from further damage in patients with VaD. - Remaining neurons could be protected.
- Promising role for patients with VaD and silent
brain infarcts.
34
Pharmacologic treatment of dementiaBehavioral
symptoms
- Behavioral symptoms occur in 85 of severe
dementia. - Agitation, hallucinations, delusion, aggression,
depression - Respond well to medications.
- Should be aggressively treated since often lead
to NHP. - Other behaviors respond better to behavioral
therapy - Wandering, repetitive questioning, withdrawal,
hiding objects, etc. - Cholinesterase inhibitors modestly improve
neuropsychiatric symptoms. - Reasonable to try them before moving to other
agents.
35
Pharmacologic treatment of dementiaBehavioral
symptoms
- Delusions and halluciantions
- Delusions present in 30 pts with severe AD.
- Early visual hallucinations think about Lewy
body dementia. - In AD atypical neuroleptics are drugs of choice
- Olanzapine
- Quetiapine
- Clozapine
- Risperidone
- SSRI may benefit behavior, not as well studied.
36
Pharmacologic treatment of dementiaBehavioral
symptoms
- Depression
- Complex relationship between depression and
cognitive impairment. - No reliable tool to measure relative contribution
of depression/dementia. - Therapeutic antidepressant trial
- SSRIs (citalopram)
- TCAs
37
Pharmacologic treatment of dementiaBehavioral
symptoms
- Aggression and anxiety
- Provoked by confusion, delusions, sleep
disturbances, depression. - Improve sleep
- Behavioral modifications
- Trazodone Reduces anxiety/aggression
particularly at night - Can be combined with SSRI for depression
- Antiepileptic drugs
- Carbamazepine
- Valproate
- Gabapentin
- Lamotrigine
- Benzodiazepines should be limited only to brief
stressful episodes.