Prsentation PowerPoint - PowerPoint PPT Presentation
1 / 17
Title:
Prsentation PowerPoint
Description:
No protecting effect of Amifostine (A) on acute toxicity of chemoradiation in ... upper normal limit of testing laboratory, SGOT, SGPT 3 times upper normal limit ... – PowerPoint PPT presentation
Number of Views:56
Avg rating:3.0/5.0
Title: Prsentation PowerPoint
1
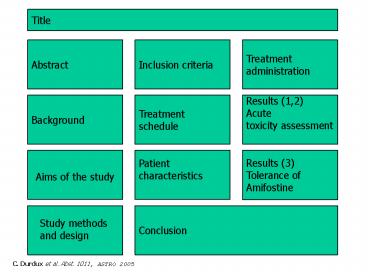
Title
Abstract
Inclusion criteria
Treatment administration
Background
Treatment schedule
Results (1,2) Acute toxicity assessment
Patient characteristics
Results (3) Tolerance of Amifostine
Aims of the study
Conclusion
Study methods and design
C. Durdux et al. Abst. 1011, ASTRO 2005
2
No protecting effect of Amifostine (A) on acute
toxicity of chemoradiation in head and neck
cancer .
- DURDUX C.1, DERRIEN G1., LEVITCHI M.1, THARIAT
J1., BRASNU D2., HOUSSET M1.1 Radiotherapy
Department 2Otorhinolaryngology Department
Georges Pompidou Hospital, Paris, France.
C. Durdux et al. Abst 1011, ASTRO 2005
3
Abstract 1011
- Purpose To evaluate the efficiency of A on
acute mucositis and skin toxicity related to
chemoradiation in head and neck cancer. - Patients and methods Between 03/01 and
03/05, 72 patients (pts) with local advanced head
and neck cancer (squamous cell carcinoma, 64 pts
undifferenciated, 5 pts, others, 3) received
chemoradiation using classical fractionation.
Tumor location was as followed nasopharynx, 5
pts oropharynx 50 larynx, 9 hypopharynx, 7
others, 3. Dose radiation exceeded 55 Gy in all
pts but 2. Concomitant chemotherapy (weekly
regimen) was cisplatin for 46 pts, carboplatin
for 17, paclitaxel for 7 and other for 2. A was
administered in a 3 minute I.V. infusion with
saline hydratation and emesis prevention. Group 1
(40 pts) received 200 mg/sqm of A before each
fraction of radiotherapy (5 days per week). Group
2 (32 pts) received 340 mg/sqm of A once a week
(chemoradiation day) and 200mg/sqm the other days
(4 days per week). No significant difference was
observed in patient characteristics between
groups 1 and 2. - Results 83 of pts received 80 of
theoretic dose of A (90 in group 1 and 75 in
group 2). Treatment was stopped in 18 pts (25)
because of hypotension (11 pts), vomiting (7) and
other (2). Grade 2 and grade 3-4 acute mucositis
were seen in 25 (62 ) and 9 (22) cases
respectively in group 1. Grade 2 and grade 3-4
acute mucositis were seen in 27 (84 ) and 2 (6)
cases respectively in group 2 (p0.11). Grade 2
radio-epithelitis was seen in 21 patients (52 )
of group 1 and 17 patients (53). Grade 3
epithelitis occurred in 3 cases (2 in group 1 and
1 in group 2). Acute xerostomia was mild in both
groups. - Conclusion In this study, A did not appear as
a radioprotector for mucositis and skin toxicity
related to chemoradiation. The study is on going
on a larger population.
4
Background
- Treatment of advanced head and neck cancers is
based on radiotherapy with concomitant
chemotherapy. - Chemoradiation results in significant acute side
effects such as mucositis and xerostomia. - Amifostine is an aminothiol prodrug converted to
the active free thiol by membrane-bound alkaline
phosphatase, effective to prevent chronic
xerostomia. - Preclinical datas demonstrated a
radiation-induced mucositis prevention by
Amifostine 1 - Recent clinical studies demonstrated Amifostine
could be useful in reducing acute mucositis and
dysphagia resulting from chemoradiation in head
and neck cancers 2,3.
5
Aims of the Study
- To explore the efficiency of 2 dose levels of
amifostine on acute toxicity observed during
chemoradiation in head and neck cancers - Primary endpoint acute toxicity of
chemoradiation - - mucositis
- - skin toxicity
- - acute xerostomia
- Secondary endpoint tolerance of Amifostine
6
Study Methods and Design
- Phase II prospective monocentric study
- Between 03/01 and 03/05, 72 patients enrolled
- - with histologically proven carcinoma of
oral cavity or pharyngo-larynx - - with who performance status lt 2
- - with adequate haematological, hepatic, and
renal function - - without metastasis
- Chemoradiation in curative intent
- Major salivary glands included in irradiated
volume (gt 55 Gy) - Radioprotection by Amifostine according to 2
dose levels - - low dose group 1 from March 2001 to December
2002 - - high dose group 2 from February 2004 to April
2005 - Clinical assessment for acute toxicity every week
from the start of therapy until 3 months after
the end of RT using RTOG scales.
7
Inclusion Criteria
- Patient selection according to the following
criteria - Histologically documented head and neck carcinoma
- WHO performance status (PS) lt 2
- Age gt 18 lt 70 years
- Adequate hematological parameters including
neutrophils gt 1,500/mm3, platelets gt
100,000/mm3, hemoglobin gt 8g/dl, serum creatinine
and total bilirubin lt 1.5 times upper normal
limit of testing laboratory, SGOT, SGPT ? 3 times
upper normal limit of testing laboratory - No prior radiotherapy
- Curative intent treatment
8
Treatment Schedule
- Radiotherapy
- 3D radiotherapy with 6 18 MV photons beams and
6-12 electrons beams - Total dose gt 55 Gy on tumor site and/or cervical
lymph nodes (areas II, III, IV, V) - Fractionation 1,8 Gy per day, 5 days a week
- Weekly Chemotherapy
- Platine derivatives
- - cisplatine 20 mg/sqm
- - Carboplatine (carbo) AUC1
- Paclitaxel 50 mg/sqm
- Protective agent Amifostine 2 groups of
patients - Group 1 Amifostine 200 mg/sqm before each
fraction of radiotherapy 5 days per week
(including days of concomitant chemotherapy) - Group 2 Amifostine 340 mg/sqm once a week
(chemoradiation day) and 200 mg/sqm the other
days (4 days per week) - Amifostine was administered in a 3 minute-IV
infusion 30 minutes before radiotherapy. - Hydratation and emesis prevention by setrons were
systematically performed.
9
Patient characteristics
- Group 1 Group 2 Total
- (40 patients) (32 patients)
(72) - Sex ratio (M/F) 31/9 26/6 57/15
- Mean age (year) 54 55
- WHO PS
- lt2 39 (98) 30 (94) 69 (96)
- Mean weight (kg) 72 70
- Histologic subtype
- UCNT 2 (5) 3 (9)
- squamous cell 35 (88) 29 (91 )
64 (89) - other 3 -
- Tumor sites
- oral cavity 5 -
- oropharynx 28 (70) 22 (69 ) 50
(70) - hypopharynx 5 2
- larynx 4 5
- nasopharynx 2 3
- others 3 -
NS
10
Treatment administration
- Group 1 Group 2 Total
- (40 patients) (32
patients) (72) - Chemotherapy (N pts)
- cisplatin 29 17
46 (64 ) - carboplatin 5 12 17
- paclitaxel 5
2 7 - carbo paclitaxel -
1 1 - cisplatin then carbo 1
- 1 - Number of cycles (mean) 7.3 1.36
7.2 1.21 NS - Radiotherapy (mean dose, Gy)
- tumeur 62 2 67 7
- cervical nodes 65 12 56
14 - Amifostine (mean dose, mg)
- days with RT alone 363 38 366
41 NS - days with RT CT - 622 70
NS
11
Results (1)
- Amifostine dose-intensity
- Number of patients received gt 80 of theoric
dose of Amifostine - N patients Group 1 Group 2 Total
- (40 patients) (32 patients)
- 36 (90 ) 24 (75) 83
- p 0.59
12
Results (2)
- Chemoradiation acute toxicity
- N patients Group 1 Group 2 Total
- (40 patients) (32 patients)
- Mucositis
- grade 1 4 3 7
- 2 25 (62) 27 (84 ) 52 (72 )
- 3 5 2 7
- 4 4 - 4
- Epithelitis
- grade 1 16 (40 ) 14 (44 ) 30
(42 ) - 2 21 (52 ) 17 (53 ) 38 (53
) - 3 2 1
- 4 - -
- No statistical significant difference between
groups 1 and 2
6
15
22
p0.11
13
Results (2)
- Chemoradiation acute toxicity
- N patients Group 1 Group 2 Total
- (40 patients) (32 patients)
- acute xerostomia
- grade 1 21 (52 ) 1 22 (30 )
- 2 15 (37 ) 30 (94 ) 45 (62
) - 3 2 - 2
- 4 - - 0
- dysgueusia
- grade 1 25 (62 ) 8 (25 ) 33
(46 ) - 2 11 (27 ) 16 (50 ) 27 (37
) - 3 1 7 (22 ) 8 (11 )
- 4 - -
14
Results (3)
- Tolerance of Amifostine
- N patients Group 1 Group 2 Total
- (40 patients) (32 patients)
- hypotension
- grade 1 - 7 (22 )
- 2 7 (17 ) 4 (13 ) 11
(15 ) - 3 - - 0
- 4 - - 0
- nausea/vomiting
- grade 1 2 11 (34 ) 13
(18 ) - 2 10 (25 ) 10 (31 ) 20 (28
) - 3 2 6 (19 ) 8 (11 )
- 4 - - 0
15
Results (3)
- Tolerance of Amifostine
- Treatment was stopped before the end of
radiotherapy in 18 patients (25 ) related to - hypotension 11 patients
- vomiting 7
- sideration 1
- patient refusal 1
- No cutaneous rash
16
Conclusions
- High dose administration of Amifostine (340
mg/sqm once a week for 6 to 8 weeks) is feasible. - Amifostine was well-tolerated with adequate
hydratation and emesis prevention for standard
administration (group 1) or high dose (group 2). - Acute xerostomia related to radiotherapy was mild
(grade 3 - 4, 2). - With 15 grade III-IV mucositis and 39 grade
II III epithelitis, Amifostine did not appear
as a radioprotector to chemoradiation. - Moreover, Grade III-IV mucositis rate could be
lower with high dose Amifostine (group 1, 22
group 2, 6) but statistical difference was not
significant (p0.11). - The study is on going on a larger population.
17
References
- Cassatt DR, Fazenbaker CA, Bachy CM, Kifle G, Mc
Carthy MP. Amifostine (Ethyol) protects rats from
mucositis resulting from fractionated or
hyperfractionated radiation exposure. Int J
Radiat Oncol Biol Phys 2005 61(3) 901 7 - Antonadou D, Pepelassi M, Synodinou M, Puglisi M,
Throuvalas N. Prophylactic use of amifostine to
prevent radiochemotherapy-induced mucositis and
xerostomia in head-and-neck cancer. Int J Radiat
Oncol Biol Phys 2002 52(3) 739 47 - Suntharalingam M, Jaboin J, Taylor R, Wolf J,
Banglore M, Van Echo D, Ord R. The evaluation of
amifostine for mucosal protection in patients
with advanced loco-regional squamous cell
carcinomas of the head and neck (SCCHN) treated
with concurrent weekly carboplatin, paclitaxel
and daily radiotherapy (RT). Semin Oncol 2004
331 (6 suppl 18) 2 7