Key to resistance to virus/bacteria infection and perhaps cancer disease - PowerPoint PPT Presentation
Title:
Key to resistance to virus/bacteria infection and perhaps cancer disease
Description:
What is Innate Immunity? Key to resistance to virus/bacteria infection and perhaps cancer disease Progression lies within the host immune system: – PowerPoint PPT presentation
Number of Views:156
Avg rating:3.0/5.0
Title: Key to resistance to virus/bacteria infection and perhaps cancer disease
1
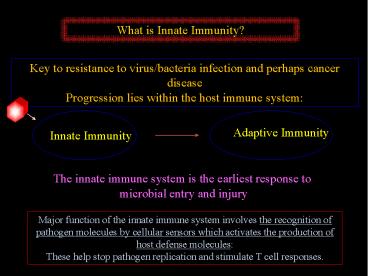
What is Innate Immunity?
Key to resistance to virus/bacteria infection and
perhaps cancer disease Progression lies within
the host immune system
The innate immune system is the earliest response
to microbial entry and injury
Major function of the innate immune system
involves the recognition of pathogen molecules by
cellular sensors which activates the production
of host defense molecules These help stop
pathogen replication and stimulate T cell
responses.
2
How important is Innate Immunity?
Very!!!!!
X
Mice defective in key innate immune response
pathways die of infection following exposure to
small amounts of virus.
The host cannot make sufficient antibody and T
cells May take up to a weektoo late..
3
Whats the difference between the innate and
adaptive immune response?
Differences between innate and adaptive immunity Differences between innate and adaptive immunity Differences between innate and adaptive immunity
Innate Immunity Adaptive Immunity
Action Time Early (hours) Late (Days)
Cell Types Macrophages, Dendritic cells, Neutrophils B, T Lymphocytes
Receptors Fixed in genomee.g., Toll-like receptor Gene rearrangement necessary e.g., B cell receptor, T cell receptor
Recognition Conserved molecular patterns e.g., LPS Wide variety of molecular structure (proteins, peptides) 1,000,000,000,000,000,000
Evolution Evolutionarily conserved (plants, animals) Only vertebrates (jawed fish-human)
4
Immune System Innate V Adaptive immunity.
5
How Does the Innate Immune Response help adaptive
immunity?
The production of cytokines referred to as the
INTERFERONS, are very important at boosting the
production of more cytokines that exert
anti-viral activity and stimulate T-cell
responses.
6
Infected Cells Produce Interferon/Cytokines.
Interferons made (by PRRs)
Phagocytes (DCs) eat dying infected cell and
PAMPS activate PRRs in phagocyte. More
cytokines are made. Antigen presentation occurs-
Adaptive immunity
Interferons protect other cells, recruit
phagocytes
7
Viruses (HSV-1) triggers innate immune gene
activation fibroblast
WT STING-/-
HSV1
8
Cellular Sensors have Evolved to Detect
Pathogens How?
PAMP- pathogen associated molecule pattern
Viruses- RNA genome, DNA genome. Bacteria-
LPS, flagella, DNA genome. DAMP- damage
associated molecular pattern Uric acid,
ROS. PRR- Pathogen Recognition Receptor
Toll-Like Receptors RLR Inflammasome
pathway (AIM2) STING Pathway.
9
Viruses have either DNA or RNA genomes.
DNA Viruses
Adenovirus Herpes Simplex Virus Vaccinia Virus
RNA Viruses
Newcastle disease virus/Measles/ Mumps. Vesicular
Stomatitis Virus/Rabies. Reovirus. Influenza virus
HIV is a lentivirus (retrovirus family) that has
a genome that exists in both RNA and DNA forms,
depending on the stage of its life cycle.
10
Virus/RNA/DNA Signaling
Isaacs and Lindemann 1958 Found interference
factors were secreted from cells in response to
flu infection. These interferons exerted
anti-viral activity. How are the interferons
activated? dsDNA/dsRNA is a very good activator
of interferon.
dsRNA and DNA
Search for dsRNA/DNA activated proteins
The Interferons Type I a/ß 148 aa
Interferon genes
11
Isaacs and Lindenmann
12
A
Viral induction of interferon
?
13
Vesicular Stomatitis Virus- VSV
Virus Vesicular Stomatitis Virus
(VSV). Negative-stranded RNA Contains only 5
genes Usually harmless to mice and
humans Generates 5 subgenomic mRNAs Lytically
infects many types of cells
Mock
VSV
Type I IFN VSV
14
Cellular Sensors have Evolved to Detect
Pathogens How?
PAMP- pathogen associated molecule pattern
Viruses- RNA genome, DNA genome. Bacteria-
LPS, flagella, DNA genome. DAMP- damage
associated molecular pattern Uric acid,
ROS. PRR- Pathogen Recognition Receptor
Toll-Like Receptors RLR Inflammasome
pathway (AIM2) STING Pathway.
15
How Did we Find Cellular PAMPs
Insects evolved over 400 million years ago
Maybe 10 million species
Insect immunity relies on three major mechanisms
Phenoloxidase Pathway synthesizes melanin at
injury site which may effect invading
microorganisms
Phagocytosis cellular arm
Humoral response best characterized
TOLL
IMD
Responses to bacteria and fungi are well
characterized Almost nothing is known about
viruses (ARBOVIRUSES)
16
(No Transcript)
17
Toll Pathway
Discovered in 1985 by Christiane
Nusslein-Volhard Drosophila- Toll weird, loss
affected drosophila development. In 1996 Jules
Hoffman showed Toll to have role in immune
response in flies in response to fungal
infection and bacteria. Pattern Recognition
Receptors (PRR) that recognize pathogen
associated molecular patterns (PAMPs). Members
of the Interleukin I receptor superfamily which
have a Toll-IL-1-receptor (TIR) domain. Nomura
and colleagues showed that Toll homologues
existed in humans. Janaway and Medzhitov showed
that TLR4 could be activated with antibody to
induce innate immune genes. Bruce Buetler proved
that TLR4 was receptor for endotoxin produced
from gram-negative bacteria Lipopolysaccharide
(LPS). Hoffman and Beutler won Nobel prize in
2011 for their work.
18
Insect Cells
19
PAMPs (Pathogen Associated Molecular Patterns
Trigger Host Defense NF?B/AP1 Gene
Induction
20
Crystal Structure
21
Which tissues express TLRs?
Mostly macrophages/monocytes
TLR1- MyD88 macrophages TLR2- MyD88
macrophages/myeloid DC TR3- TRIF DCs, B
lymphocytes TLR4- MyD88/TRIF macrophages/myeloid
DC, intestinal epithelium. TLR5-
MyD88 macrophages/myeloid DC, intestinal
epithelium. TLR6- MyD88 macrophages, B
lymphocytes TLR7- MyD88 macrophages, B
lymphocytes, pDCs TLR9- MyD88 macrophages TLR9-
MyD88 macrophages, pDCs, B-lymphocytes.
HIV infects many of these cell types
22
HIV-mediated TLR Signaling in pDCs
23
Is innate Signaling Involved in Cytokine
Production during Acute HIV Infection?
cytokines
Probably- but difficult to test
experimentally, Is STING involved in suppressing
HIV Infection during latency?
24
Inhibitory Cytokines Involved in HIV-1 Infection
Inhibitory Cytokine Produced by Cell Targeted Mode of Action
IFN-a Leukocytes and dendritic cells9 T cells, monocytes, macrophages Inhibits replication of HIV-1 by suppressing reverse transcriptase.9
IL-10 Monocytes, macrophages, T cells, and B cells21 Macrophages21 Inhibits replication of HIV-1 in the early stages of infection. Inhibition is associated with its ability to down-modulate production of IL-6 and TNF-a21.
IL-13 Dendritic cells and T cells Macrophages21 Inhibits HIV-1 infection and production by down-modulating CCR5 expression on macrophages, blocks revers transcription, and suppresses HIV-1 replication at the post-transcriptional level.9
IL-16 T cells, mast cells, eosinophils9 CD4 T cells9 IL-16 is a natural ligand for the CD4 receptor, so it inhibits HIV-1 entry into CD4 T cells1,9
25
Stimulatory Cytokines Involved in HIV-1 Infection
Stimulatory Cytokine Produced by Cell Targeted Mode of Action
TNF-a Monocytes, macrophages,T cells, B cells, NK cells, and neutrophils 9 Monocytes and macrophages Powerful activator of transcription factor NF-?B.2122 9Activation of NF-?B is followed by nuclear translocation and binding to HIV long-terminal repeat (LTR), which leads to initiation or increases in viral transcription22.
M-CSF Fibroblasts and endothelial cells21 Macrophages21 Stimulates increased surface expression of CD4 and CCR5 receptors. Results in greater HIV-1 entry and replication.21
IL-1 Monocytes, macrophages, and neutrophils9 Monocytes and macrophages9 Upregulates HIV-1 viral replication in infected monocytes and macrophages. Stimulates HIV-1 expression in U1 latently-infected cells9
IL-6 T cells, B cells, and macrophages21 Monocytes and macrophages9 Synergizes with TNF-a to stimulate HIV expression in latently infected cell lines. Potentiates TNF-a-induced HIV-1 production and transcription of NF-?B.9
IL-12 Macrophages and dendritic cells9 T cells9 Stimulates HIV-1 replication in peripheral blood mononuclear cells (PBMC), CD4 T cells, and T cell lines. It also triggers IFN-? production. 9
26
What is known about HIV and the Toll-Like
Receptor Pathway
HIV may infect dendritic cells and trigger TLR 7
or other sensors. Type I IFN is produced to help
fight infection. However, the virus can also
upregulate TRAIL (TNF-related apoptic ligand) on
the DCs. This can bind to TRAIL receptors on
CD4 cells and induce CD4 depletion!
So, Yes, the TLR pathway is engaged (TL7), but
its influence on AIDS has yet to be clarified
Atfield and Gale, Nature Immunology Vol 16, June
2015
27
TLRs in host defense
Activation of the TLRs leads to up regulation of
100s of genes. Required for immune responses to
pathogens- not essential in many cases. Over
activation can lead to inflammation.
Autoimmunity? Pathogens/necrosis? Role in
inflammatory bowel disease- Therapeutic
intervention? CD destruction and opportunistic
disease. TB, AND OTHER BACTERIA.. BUT,
development of knock out mice indicated that
animals lacking TLR3 or 9 Still made IFN in
response to viral infection.. THUS, other
sensors must exist in addition to the TLR pathway.
28
Discovery of the RIG- Pathway, 2004 Fujita
1 200 300 400 500 600
700 800 900
MDA-5
1
1025
RIG-I
925
1
CARD/ Death-like
RNA Helicase
DEAD BOX
LGP2e
1
678
29
RIG-I and MDA5 Evolved to Detect Viral RNA Species
30
What is known about HIV and RIG-I and MDA5?
TLR 7 is more important in pDCs than the RIG-I
like pathway. pDCS ARE high level type I IFN
producers Other cells could make
interferon/cytokines in response to HIV
infection and be RIG-I/MDA5 specific. Little
data exists in vivo to implicate MDA5/RIG-I
pawthay so far! But purified HIV RNA can
activate signaling.
31
Pattern Recognitions Receptors
32
Overexpression of STING activates IFN. STING is
localized to the ER (translocon). STING is
expressed in Dendritic cells,
macrophages, endothelial cells, epithelial cells.
STING STimulator of
INterferon Genes
1
379
Transmembrane regions.
Peripheral leukocyte
Small Intestine
Skeletal muscle
Placenta
Spleen
Kidney
Thymus
Liver
Lung
Brain
Heart
Colon
2.4 -
hSTING
1.35 -
lung
ß-actin
Ishikawa and Barber Nature 2008
33
Viruses (HSV-1) triggers innate immune gene
activation fibroblast
WT STING-/-
HSV1
34
c-GMP-AMP (cGAMP) synthase -cGAS
DNA ATP, GTP
mAb21 domain
2-5- cyclic dinucleotides
1
522
NTase core
Side and top views of cGASMab21 in complex with
dsDNA (brown), GTP and ATP (ruby stick models).
DNA binds along the platform between spine and Zn
thumb. b, Close-up view of the DNA binding site
with selected annotated residues. DNA is bound
mainly via the minor groove. A notable exception
is the Zn thumb near the major groove. c,
Schematic representation of DNAcGAS contacts.
Civril et al., Nature, 2013.
35
STING is a sensor for cyclic dinucleotides
2011
Shang et al., Nat Struc Mol Biol, 2012
Cyclic GMP-AMP synthase is a cytosolic DNA
sensor Sun et al., Science 2013
36
Is STING Signaling Involved in Cytokine
Production during Acute HIV Infection?
cytokines
Probably- but difficult to test
experimentally, Is STING involved in suppressing
HIV Infection during latency?
37
HIV Does it activate STING Signaling?
38
Innate Immunity activated here?
39
Does HIV Trigger STING activity and Innate Immune
Signaling?
STING signaling triggered here?
40
What is known about cGAS/STING and Sensing HIV
Infection?
Cyclic GMP-AMP Synthase Is an Innate Immune
Sensor of HIV and Other Retroviruses. Gao et al.,
SCIENCE, 2013.
The capsids of HIV-1 and HIV-2 determine immune
detection of the viral cDNA by the innate
sensor cGAS in dendritic cells. Lahaye et al.,
IMMUNITY, 2013.
Cytosolic RNADNA hybrids activate
the cGAS-STING axis. Mankan et al., EMBO J, 2013.
Nucleic acid recognition orchestrates the
anti-viral response to retroviruses. Stavrou et
al., CELL HOST MICROBE, 2015.
PQBP1 Is a Proximal Sensor of the cGAS-Dependent
Innate Response to HIV-1. Yoh et al., CELL 2015.
Viruses transfer the antiviral second messenger
cGAMP between cells. Bridgeman et al., SCIENCE,
2015.
Sequence-specific activation of the DNA sensor
cGAS by Y-form DNA structures as found in primary
HIV-1 cDNA. Herzner et al., NATURE IMMUNOLOGY
2015.
41
Why doesnt STING or other innate immune pathways
clear HIV infection?
Maybe they do in some instances. Maybe cytokine
production can facilitate HIV replication. Masyb
e the STING or other innate immune signaling
pathways are suppressed by HIV? Latency?
Re-emergence? T-cell depletion?
papers
42
Atfield and Gale, Nature Immunology, 2015.
43
How Can Our Understanding of Innate Immunity Help
Prevent HIV/AIDS?
Understanding whether HIV inhibits these pathway
may enable the design of drugs that block this
virus/host interaction. Such drugs may prevent
efficient HIV replication. Understanding these
pathways helps us design new ways to stimulate
the immune system Adjuvants, Vaccines. RIG-I/MD
A5 agonists (polyIC), TLR agonists (imiquimod)
STING agonists (cyclic- dinucleotides). Opportun
istic infections are a key problem, so
understanding how the innate immune system is
regulated by microbes may help us combat these
diseases. HHV8, EBV, HPV, bacteria
(tuberculosis), fungi. STING agonists exert
potent anti-tumor ability and so may be helpful
against AIDS related malignant disease.
44
NOD-like Receptors
TLRs recognize PAMPS (LPS etc) Nucleotide-bindin
g oligomerization domain-NOD receptor family
(NLR) are also important for recognizing
bacteria- results in an inflammatory
response. Mediated by the induction of IL-1beta,
IL6 and TNF alpha. NLR family has approx 22
members. Primarily expressed in immune cells,
lymphocytes and APCs, Macrophage, DCs also in
epithelial cells and mesothelial cells. They
have a variety of domains- CARD, PYD etc. Three
major activation targets are not IFN but NF-kB,
MAPKs and caspase-1. NOD family recognize NF-kB
and MAPKs, NALP (NACHT-LRR-PYD)-
inflammasome. NODs compliment the TLRs- for
effective immunity.
45
NOD-like Receptors II-Recognition of ligands
Individual NLRs have been shown to be important
against specific pathogens for example, Nod1 and
Nod2 recognize peptidoglycan (PGN) moieties found
in bacterial cell wall that are secreted by the
bacteria. However, a direct interaction between
a putative ligand and its corresponding NLR has
not been shown for most Nods- perhaps
intermediary host factors exist? NOD1/NOD2
recognize peptidoglycan (PGN), major component of
bacterial cell wall activates NF-kB and
MAPK pathways. NLRC5 (NOD27) regulates
antiviral innate and adaptive immunity through
the induction of inflammatory
cytokines- NF-kB. Unknown ligand. Secretion
system in bacteria makes pores in host cell and
introduces virulence factors that activate NLRs
(secretion system III and IV).
46
PRRS-NOD-like receptors (NLRs) and
inflammasomes.
CARD
inflammasomes
FIIND
LRR
LRR
NAD
NACHT
NACHT
PYD
Pyrin dom
CARD
NODs
NALPs
IPAF/NAIP
Nucleotide-binding oligomerization
domain-NOD Epithelial cells- bacterial
muropeptides- NF-kB
PAMPS (PGN, cytosolic DNA), ROS, K efflux LRR-
ligand recognition, PYD-PYD association and
oligomerization of NACHT domain into high
molecular weight complexes. Recruits ASC
(apoptosis-associated speck-like protein
containing a CARD), then caspase-1. Targets
substrates IL-1 beta and IL-18- active IL-1R and
IL-18R- MyD88 pathway. Activates inflammatory
responses acts as an autocrine adjuvant to
upregulate co-stimulatory molecules?.
47
Pattern Recognitions Receptors
48
NOD aggregation and inflammasome activation
49
Recognition of RNA and RNA Viruses by
RIG-Like-Receptors (RLRs).
50
NOD-like Receptors III-Inflammasomes
NLRP1 MDP NLRC4 virulence factors NLRP3- DAMPs-
directly or indirectly Non NLR- AIM
III Recognize DAMPs directly or indirectly All
activate caspase I in response to a wide variety
of bacteria TLRs and NODs co-operate to fight
infection. Recognize bacteria that escape TLRs,
that invade intracellulary that are engulfed.
51
Recognition of DNA Viruses DNA Pathogens
52
Host Defense Genes / Development
53
Type I IFNs-dependent innate immunity
Virus infection
IFN
nucleic acids
IFNR
JAK-STAT signaling
Sensor
Anti-viral genes
Signaling
Type I IFN (IFNa, IFNb)
54
PAMPS Recognized by the TLRs and their Adaptors