Case%20Report - PowerPoint PPT Presentation
Title:
Case%20Report
Description:
Case Report 39-year-old white male, diagnosed with Rf+ rheumatoid arthritis at the age of 17, presented to his primary care physician with shortness of breath and ... – PowerPoint PPT presentation
Number of Views:224
Avg rating:3.0/5.0
Title: Case%20Report
1
Case Report
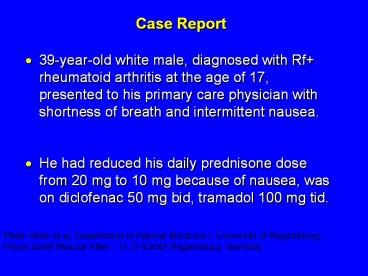
- 39-year-old white male, diagnosed with Rf
rheumatoid arthritis at the age of 17, presented
to his primary care physician with shortness of
breath and intermittent nausea. - He had reduced his daily prednisone dose from
20 mg to 10 mg because of nausea, was on
diclofenac 50 mg bid, tramadol 100 mg tid.
Peter Härle et al, Department of Internal
Medicine I, University of Regensburg,
Franz-Josef-Strauss-Allee , 11,
D-93042 Regensburg, Germany
2
- In addition to steroid therapy, several different
disease-modifying drugs were given over the years
since diagnosis, including sulfasalazine, oral
gold, chloroquine, methotrexate, and
TNF-inhibitors. - A total of 16 orthopedic operations had been
performed including excision of rheumatic
nodules, tendon repair, and bilateral knee- and
unilateral hip-replacement.
3
- On exam, he showed signs of extensive rheumatoid
arthritis, most marked on hand, foot, and
shoulder joints as well as rheumatic nodules on
both elbows. - HR regular at 105/min
- BP 130/90 mm Hg
- ESR 82 mm/h
4
- A CT-scan and echo revealed a pericardial
effusion (1.5 cm), a thickened pericardium
(5 mm), and basal bilateral low-grade lung
fibrosis. - Diuretic therapy and increased prednisone dose
controlled his symptoms - The pericardial effusion was almost undetectable
4 weeks later.
5
- Four months later, he was admitted to the
hospital because of a sudden onset of abdominal
pain. - A perforated NSAID/steroid-induced ulcer was
diagnosed and the patient required emergency
surgery. - During anesthesia, severe cardiovascular problems
developed including low blood pressure,
tachycardia, and pre-renal kidney failure. - A left and right heart catheterization was
performed subsequently which showed a cardiac
index of 2.4 l/min/m2, equalization of elevated
left and right ventricular diastolic pressures.
6
- Coronary angiography revealed a 75 obstruction
of the diagonal branch. - An MRI-scan showed a thickened pericardium
(5 mm), a small pericardial effusion, enlarged
right atrium, and bilateral pleural effusions.
7
- Patient was diagnosed with constrictive
pericarditis without a hemodynamic relevant
pericardial effusion. - He was referred to CT Surgery
- Pericardectomy was suggested.
- The patient was informed about the prognosis of
this RA-associated complication but declined
surgery and was discharged in improved physical
condition.
8
- Repeated hospitalizations were necessary because
of clinically dominant right heart failure. - On his last admission, p/w cachexia, extensive
edema, tachycardia of 122/min, blood pressure of
105/55 mm Hg, orthopnea, and ascites. - Follow-up heart catheterization revealed a
reduced ventricular function with a cardiac index
of 1.46 l/min/m2.
9
- Surgical intervention was recommended repeatedly
but the patient still declined any further
procedures. - In the following weeks, the patient had three
episodes of renal failure attributable to low
median blood pressure (4060 mm Hg) together with
diuretic therapy - Intermittently required vasopressor medication.
- The CT-scan of the chest did not show a
hemodynamically relevant pericardial effusion.
10
- Fig. 1. This CT-scan was conducted without
contrast because of recurring prerenal kidney
failure. A thickened pericardium (5 mm) could be
seen next to a small pericardial and bilateral
pleural effusion. The pericardial effusion did
not seem to be of hemodynamic relevance
11
- Pt was noted to be adrenally insufficient and
have pancreatic insufficiency - In the following weeks, cardiovascular and renal
functions were increasingly difficult to
stabilize and intermittent dialysis was
necessary. - He developed a DVT despite the use of
prophylactic heparin and a bilateral pneumonia
despite broad-spectrum antibiotic therapy. - The patient died in septic shock combined with
multi-organ failure.
12
- The patient died 2 years after the onset of
extra-articular cardiac symptoms. - Pericarditis is a frequent extra-articular
manifestation of rheumatoid arthritis showing a
post-mortem prevalence of 3050. - These findings correlate well with
echocardiographic diagnosis in living patients.
However, clinically relevant symptoms are rare
with a prevalence of 0.063 of all RA patients - This case demonstrates the devastating course of
progressive constrictive pericarditis under sole
medical therapy and emphasizes the importance of
early radical pericardectomy to avoid progression
of disease and secondary complications with fatal
outcome.
13
Rheumatoid ArthritisJulie Schwartzman, MD
14
Rheumatoid Arthritis
- A systemic, inflammatory polyarthritis that leads
to joint destruction, deformity, and loss of
function - Several potentially severe extra-articular
manifestations - Pathology of RA involves the synovial membranes
and periarticular structures of multiple joints,
resulting in - Pain
- Swelling
- Stiffness
- Uncontrolled inflammation that can lead to
irreversible damage and deformity - Functional limitation
ACR Subcommittee on RA Guidelines. Arthritis
Rheum. 200246328346 Goronzy JJ, Weyand CM.
In Klippel JH, et al, eds. Primer on the
Rheumatic Diseases. 12th ed. Atlanta, GA
Arthritis Foundation 2001209217 Anderson RJ.
ibid. 218225 Arnett FC, et al. Arthritis Rheum.
198831315324.
I.2
15
ACR 1987 Classification Criteria For Rheumatoid
Arthritis
- Patients Must have Four of Seven Criteria
- Morning Stiffness Lasting at Least 1 Hour
- Swelling in 3 or More Joints
- Swelling in Hand Joints
- Symmetric Joint Swelling
- Erosions or Decalcification on X-Ray of Hand
- Rheumatoid Nodules
- Abnormal Serum Rheumatoid Factor
- Must Be Present at Least 6 Weeks
16
Epidemiology of RA
- Prevalence 0.5 - 2
- 2 3 times more prevalent in women
- Increased prevalence with advancing age
- 100,000 200,000 New Cases/yr
- 4 6 million current cases of RA
17
Mode of Onset
- Monoarticular 21
- Oligoarticular 44
- Polyarticular 35
18
Site of Onset
- Joint Involvement
- MCP, PIP
- Wrist
- Knees
- Shoulders
- Ankles
- Feet
- Elbows
- Hips
- Mean of Patients
- 91
- 78
- 64
- 65
- 50
- 43
- 38
- 17
19
Course of Disease
- Clinical remission 10
- Intermittent 15 - 20
- Progressive 70 - 75
20
(No Transcript)
21
(No Transcript)
22
(No Transcript)
23
(No Transcript)
24
(No Transcript)
25
(No Transcript)
26
(No Transcript)
27
(No Transcript)
28
(No Transcript)
29
(No Transcript)
30
(No Transcript)
31
(No Transcript)
32
Extra-articular Manifestations of Rheumatoid
Arthritis
33
(No Transcript)
34
(No Transcript)
35
(No Transcript)
36
Sceritis
37
Secondary Sjögrens Syndrome
- SICCA
- Pleuritis/ Pericarditis
- Ro/La positive
- Hypergammaglobulinemia
38
(No Transcript)
39
(No Transcript)
40
Vasculitis
- Digital vasculitis
- Cutaneous ulceration
- Peripheral neuropathy
- Mononeuritis multiplex
41
(No Transcript)
42
(No Transcript)
43
Pulmonary Involvement
- Pleural Disease
- Interstitial fibrosis
- Nodules
- Pneumonitis
44
(No Transcript)
45
Cardiac Involvement
- Pericarditis
- Myositis
- Endocardial Inflammation
- Conduction Defects
46
Articular Manifestations Synovial Fluid Analysis
- Straw colored to slightly cloudy
- WBC 5000 25,000/ mm3
- Rheumatoid Factor
- Elevated protein
- Decreased glucose
47
Laboratory Presentation
- Leukocytosis
- Eosinophilia
- Thrombocytosis
- Mild Anemia
- ESR gt 30 mm/hr
- Normal renal and hepatic function
- Negative ANA
- Rheumatoid Factor
48
Anti-Cyclic Citrullinated Peptide(CCP)
Antibodies
- High diagnostic specificity (gt98) and
sensitivity - Presence in 65 of early RA, with the same
specificity - Prognosis value linked to the most erosive forms
49
Differential Diagnosis
- Infectious Arthritis
- Thyroid Disease
- Malignancies
- Polymyalgia Rheumatica
- Hemochromatosis
- Seronegative polyarthritis
- Psoriatic Arthritis
- Reiters Syndrome
- Chondrocalcinosis
- Gout
- Behcets Syndrome
50
Baseline Evaluation
- 43 yo AAF came to PMD, reports 4 mo. h/o
bilateral wrist and knee pain. - Occasional swelling in wrists and knuckles
- No PMH
- Takes tylenol for pain w/o relief
- BASELINE EVALUATION
- Important questions
51
Baseline Evaluation of Patients
- Subjective/History
- Degree of joint pain/swelling symmetry? joints
involved? - Presence/Duration of morning stiffness
- Presence of fatigue
- Limitation of function
- H/o SICCA symptoms? Recent GI/GU infection?
Sexual Activity?
52
Baseline Evaluation of Patients
- Physical Exam
- Essential Assessments
53
Baseline Evaluation of Patients
- Physical Examination
- Documentation of actively inflamed joints
- Documentation of mechanical joint problems loss
of motion, crepitus, instability, deformity - Documentation of extra-articular manifestations
- Optho, cardiac, pulmonary, rash, LAD
54
Baseline Evaluation of Patients
- LABS/STUDIES
55
Baseline Evaluation of Patients
- Laboratory
- ESR /C-reactive protein
- Rheumatoid factor/Anti-CCP Ab
- ANA, Subserologies?
- Complete blood cell count
- Renal function and electrolytes
- Hepatic panel
- Urinalysis
- Synovial fluid analysis
- Consider HIV, Uric Acid
56
Baseline Evaluation of Patients
- Radiography
- Wrist and hands
- Feet
- Other symptomatic joints
57
Rheumatoid Arthritis Classification of Function
- Class I No Limitations
- Class II Adequate for Normal Activities
Despite Joint Discomfort or
Limitation of Movement - Class III Inadequate for Most Self-Care and
Occupational Activities - Class IV Largely or Wholly Unable to
Manage Self-Care Restricted to Bed or
Chair
58
ACR20/50/70/90 Response Criteria
- A 20, 50, or 70 or 90 improvement in
- Swollen joint count, AND
- Tender joint count, AND
- At least three of the following
- Patients global assessment of disease activity
- Physicians global assessment of disease activity
- Patients assessment of pain
- Acute-phase reactants (ESR or CRP)
- Patients assessment of disability (HAQ)
Felson DT, et al. Arthritis Rheum.
199538727735 Felson DT, et al. Arthritis
Rheum. 19984115641570.
59
Health Assessment Questionnaire (HAQ)
- Widely accepted, validated, rheumatology-specific
instrument to assess physical function in RA - Gold standard
- 20 questions covering 8 activities
- Dressing and grooming, arising, eating, walking,
hygiene, reaching, gripping, activities of daily
living
OMERACT Outcome Measures in Rheumatoid
Arthritis Clinical Trials
Buchbinder R et al. Arthritis Rheum.
1995381568-1580. Sullivan FM et al. Ann Rheum
Dis. 198746598-600.
60
Disease Activity Score 28 (DAS28)
Assessment of Improvement or Response
DAS28 0.56 ?(t28) 0.28 ?(sw28) 0.70
Ln(ESR) .014GH
- t28 number of tender joints among 28 joints
- sw28 number of swollen joints among 28 joints
- ESR erythrocyte sedimentation rate (mm/hour)
- GH general health status using a 100-mm
visual analog scale (VAS)
High disease activity ? 5.1, low disease activity
? 3.2, remission ? 2.6
DAS28 Simplified disease activity score Prevoo
ML, et al. Arthritis Rheum. 1995384448.
61
Sharp Scores of Radiographic Progression
- Erosion scores
- 17 joints of each hand/wrist
- 6 joints of each forefoot
- Scale 05 Total score 0230
- Joint space narrowing (JSN) scores
- 16 joints of each hand/wrist
- 5 joints of each forefoot
- Scale 04 Total score 0168
- Total Sharp score
- Add erosion and JSN scores
- Total score 0398
Sharp JT, et al. Arthritis Rheum.19852813261335
van der Heijde DM, et al. J Rheumatol.
19952217921796.
62
Prognostic Markers in RA
- Early Markers
- Generalized onset with numerous joints involved
- Systemic involvement including fatigue, fever,
weight loss, morning stiffness - Elevated CRP or ESR
- Positive test for rheumatoid factor/Anti-CCP
- Early erosions, JSN
- HLA-DR4 genetic marker
63
Prognostic Markers in RA
- Later Markers
- Involvement of more joints
- Increased morning stiffness
- Rheumatoid factor 1160 or greater
- Anemia and thrombocytosis
64
Prognostic Markers in RA
- Definitive Markers
- Subcutaneous nodules
- Detection of erosions on x-ray
65
The Importance of Early Diagnosis
- RA is progressive, not benign
- Structural damage and disability occurs within
first two to three years of disease - Slower progression of disease is linked to early
treatment with DMARDs, Biologic Agents
66
RA Progression
Severity (arbitrary units)
0
5
10
15
20
25
30
Duration of Disease (years)
Adapted from Kirwan JR. J Rheumatol.
200128881886.
I.6
67
Joint Erosions Occur Early in RA
- Up to 93 of patients withlt2 years of RA may
have radiographic abnormalities - Erosions can bedetected by MRI within 4 months
of RA onset - Rate of progression is significantly more rapid
in the first year than in the second and third
years
Maximum Joints Affected
Hand
MTP
All
Year
Fuchs HA et al. J Rheumatol. 198916585-591. McQu
een FM et al. Ann Rheum Dis. 199857350-356. van
der Heijde DM et al. J Rheumatol.
1995221792-1796.
68
Treatment The Earlier the Better
Delayed Treatment(median treatment lag time
123 days n 109) Early Treatment (median
treatment lag time 15 days n 97)
14
12
10
8
Change in Median Sharp Score
6
4
2
0
0
6
12
18
24
Time (months)
Patients were treated with chloroquine or
azathioprine. Lard LR, et al. Am J Med.
2001111446451.
I.16
69
The Goals of Treatment
- Eliminate synovitis and disease activity
- Improve symptoms
- Prevent joint damage
- Prevent or reduce disability
- Prevent or reduce other adverse outcomes
Adapted from Wolfe F et al. J Rheumatol.
2001281423.
70
Current Treatment Options
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- Corticosteroids
- Disease Modifying Anti-rheumatic Drugs (DMARDs)
- Biologic Agents
71
Potential Toxicity of NSAIDs
- COX-1
- Gastrointestinal toxicity
- Platelet dysfunction
- COX-1 and COX-2
- Decreased renal blood flow
- Hepatic dysfunction
- CNS toxicity dizziness, tinnitus, confusion,
anxiety - Hypersensitivity
- COX-2
- Increased risk of cardiovascular disease
- Increased risk of thrombosis
72
Traditional DMARDs
- Cyclosporine
- Parenteral/oral gold
- Azathioprine
- D-penicillamine
- Minocycline
- Methotrexate (MTX)
- Hydroxychloroquine
- Leflunomide
- Sulfasalazine
Not approved by the FDA for the treatment of
RA. ACR guidelines for the management of
rheumatoid arthritis. Arthritis Rheum.
200246328-346.
73
Methotrexate - Dosage
- Initiation 7.5 mg once weekly
- Maximum 25 mg once weekly
- Route po, SQ
74
Methotrexate - Potential Toxicity
- Hematologic
- Teratogenic
- ?Carcinogenic
- Stomatitis
- Alopecia
- Pulmonary
- Hepatic- check LFTS q 6 weeks then q 3 mo when on
stable dose
75
Leflunamide - Arava
- Can be given with loading dose 100mg qd x 3 days,
then 10-20mg po qd - Monitor CBC, LFTs
- Teratogenic
- Cholestyramine is given if rapid removal is
necessary
76
Antimalarials
- Hydroxychloroquine - plaquenil
- Initiation 400 600 mg qd
- Maintenance 200 mg qd
- Chloroquine
- Initiation 500 mg qd
- Maintenance 250 mg qd
- Potential Toxicities GI, Retinopathy
77
Sulfasalazine
- Dosage
- 2 3 gm qd in 2 3 divided doses
- Potential toxicity
- Hematologic
- Monitor CBC q2 weeks the first 3 months of
therapy - Hepatic
- Monitor hepatic function monthly
78
Inhibition of Cytokines
Adapted with permission from Choy EH, Panayi GS.
N Engl J Med. 2001344907916.
79
TNF Blocking Therapies
Etanercept Infliximab
Adalimumab Characteristic (ENBREL?) (REMICADE?
(HUMIRA) Class sTNFR TNF MAb
TNF MAb Construct Recombinant Chimeri
c MAb Recombinant fusion protein
human
MAb Half-life 4 days 810 days
1020 days Binding target TNF/LT?
TNF TNF Administration 50 mg 310 mg/kg 40
mg SC IV with MTX SC Once weekly Every 48
weeks Every other week
Some patients not taking concomitant MTX may
derive additional benefit fromincreasing the
dosing frequency of adalimumab to 40 mg every week
80
(No Transcript)
81
- Rituximab (chimeric murine-human anti CD20 Ab)
- in combination with methotrexate is indicated
to reduce signs and symptoms in adult patients
with moderately- to severely- active rheumatoid
arthritis who have had an inadequate response to
one or more TNF antagonist therapies.
82
Figure 2 B-cell functions are inhibited following
cell depletion by rituximab
Salama AD and Pusey CD (2006) Drug Insight
rituximab in renal disease and transplantation Nat
Clin Pract Neprol 2 221230 doi10.1038/ncpneph0
133
83
Abatacept CTLA-4Ig
84
ACR Treatment Algorithm
RHEUMATOLOGIST
Establish diagnosis of RA early
PCP
Initiate therapy
Periodically assess disease activity
Adequate response
Inadequate response
Change/add DMARDs
Suboptimal MTX response
MTX naïve
Othermonotherapy
Combination
Biologics
Othermonotherapy
Combination
MTX
Monotherapy
Combination
Multiple DMARD failure
Symptomatic and/or structural joint damage
Adapted from ACR guidelines for the management
of rheumatoid arthritis. Arthritis Rheum.
200246328-346.
84
85
- Questions
- Case report
86
Case Report
- 57-year-old man was admitted to a hospital
affiliated with dyspnea and dry cough lasting 2
weeks. - He had previously been diagnosed with rheumatoid
arthritis, manifested by painful swelling of the
joints 2 years prior to admission. - The patient was being treated with prednisone and
gold. - Patient with diffuse pulmonary rheumatoid nodules
and interstitial fibrosis throughout both lungs,
is described. - The patient, with articular symptoms and
seropositivity, exhibited a rapid clinical course
and died of respiratory failure 3 months after
the appearance of dyspnea.
87
(No Transcript)
88
(No Transcript)
89
(No Transcript)
90
(No Transcript)
91
- Chest radiography indicated interstitial
pneumonitis with bilateral diffuse peripheral
shadows. - At autopsy, numerous rheumatoid nodules and
interstitial fibrosis had destroyed both lungs,
such that no residual normal pulmonary tissue
remained. - It is believed that this was an extremely rare
case exhibiting large numbers of rheumatoid
nodules throughout the lungs. - Findings with this patient indicate that, in
patients with rheumatoid arthritis, clinical
interstitial pneumonitis confirmed
radiographically does not exclude the existence
of rheumatoid lung nodules.