Rhythms in Labour 3rd Stage PowerPoint PPT Presentation
1 / 20
Title: Rhythms in Labour 3rd Stage
1
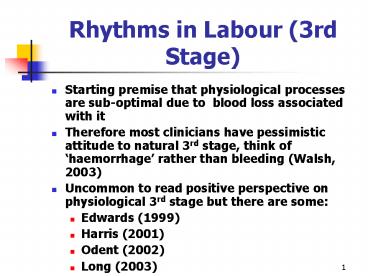
Rhythms in Labour (3rd Stage)
- Starting premise that physiological processes are
sub-optimal due to blood loss associated with it - Therefore most clinicians have pessimistic
attitude to natural 3rd stage, think of
haemorrhage rather than bleeding (Walsh, 2003) - Uncommon to read positive perspective on
physiological 3rd stage but there are some - Edwards (1999)
- Harris (2001)
- Odent (2002)
- Long (2003)
2
History of Oxytocics (den Hertog et al, 2001)
- Ergot known about since 1582 but use discontinued
in 1828 because of uterine rupture and fetal
death - Oxytocin described first in 1954 and use has
increased since that time - PPH major cause of maternal death in developing
world and WHO recommends routine oxytocic use - Research reviews indicated
- prophylactic oxytocics reduced PPH by 40
- syntometrine maybe drug of choice v ergot,
syntocinon, prostin
3
Contextualising Issues for 3rd Stage
- Historical concerns with impact of 500ml blood
loss needs updating (public health and affluence
of population moved on since 1960s) - 500 ml threshold not clinically significant for
most women in the developed world - Assembly line birth requires rapid completion of
labour stages - Routine use of oxytocin part of medicalisation of
childbirth since hospitalisation of birth - Do the results of RCTs inform
- care in midwife-led birthing suites?
- home birth?
4
Active Management
- Prophylactic oxytocics
- Early cord clamping cutting - within 2 minutes
of birth - /- Wait for signs of separation
- Delivery by controlled cord traction
5
Physiological 3rd Stage
- Watchful waiting (up to at least 1 hour midwife
retires to background) - Delivered by maternal effort gravity
- Cutting of cord after delivery of placenta
- Breast feeding, skin to skin, prioritise
mother/parent baby connection - Therefore
- not managed
- mother births placenta herself
- no oxytocic prophylaxis
6
Bristol Trial (Elbourne, 1996)
- Active v physiological management
- Hypothesis
- active reduce PPH rate from 7.5 to 5 sample
size 3900 - Stopped because of level of PPH in physiological
group
7
Bristol Trial Criticisms
- Definition of physiological approach flawed
- Some did not have physiological 1st 2nd stages
- Some of known risk for PPH were still included in
trial - Midwife practice non-compliant with physiological
approach - Definition of PPH accuracy of measurement
8
Hinchinbrook Trial (Rogers et al, 1998)
- Midwives skilled at physiological management
- Results confirm higher PPH rate
- 14 v 5 (500-999 ml) significant
- 3 v 2 (1000 ml) non significant
- numbers needed to treat (NND)
- 48 i.e. prevent 1 blood transfusion in every 48
cases
9
Hinchinbrook Trial
- Best position
- active - semi recumbent
- physiological - upright
- Other issues (Rogers Wood, 1999)
- definition of PPH
- syntocinon is oxytocic of choice
10
Active v Physiological (Prendiville et al, 2005)
- 4 RCTs
- Active management better
- blood loss
- PPH rate
- length of 3rd stage
- p/n anaemia
- Worse with ergotmetrine
- nausea/vomiting
- hypertension
11
Syntometrine v Oxytocin (McDonald et al, 2005)
- 6 RCTs
- syntometrine assoc. with significant reduction of
PPH compared with oxytocin 5 units - less so with oxytocin 10 units
- no difference with blood loss gt 1000ml
- worse nausea/vomiting/raised BP
- higher retained placenta rates (Elbourne et al,
2004) - may reduce duration of breast feeding (Begley,
1990)
12
Lente Trial in Holland (Herschderfer, 1999)
- Ongoing trial, but preliminary results available
- Community setting of independent midwifery
practices - Defined PPH as 1000 mls
- Used as marker of clinical significance transfer
for acute care - No difference between 2 groups
13
Rationale for Physiology Maternal Effects
- Reverse haemodilution of pregnancy (Harris, 2001)
- Flush out placenta
- Cleanse uterine cavity
- Umbilical attachment facilitates
- skin-to-skin, breast feeding, less crying
(Anderson et al, 2005) - emotional connection
- (Finigan Davies, 2005)
- Blood loss over 24-36 hours evens out between
both methods? (Wickham, 1999)
14
Rationale for Physiology Fetal Effects (Long,
2003)
- Delayed cord cutting means fetus slowly and
gently adapts to extra-uterine life - breathing may be delayed beyond 1 minute
- Less transfusion intraventricular bleeding in
pre-term (Rabe et al, 2005) - Conversely, early cutting starves baby of oxygen,
forcing early breathing/crying efforts - Leaving cord intact allows for physiological
transfer of blood, appropriate for babys blood
volume, neither under-transfusing or
over-transfusing (Mercer Skovgaard, 2002) - Conversely, early cord cutting combined with
oxytocic can result in under or over transfusing
15
Psycho-Social Factors
- Physiological
- woman partner can be left with their baby
uninterrupted after birth - should be completed in up to 1-2 hours
- Active
- immediate intervention after birth
- completed much earlier
- Implications for bonding (Odent, 2002)
- Implications for breastfeeding
16
Haemorrhage or Normal Bleeding?
- Why stipulate an amount at all?
- Treat on basis of clinical signs symptoms
- Individualise assessment i.e. any predisposing
risks for 3rd stage, challenge spurious ones like
grand multiparity (Page, 2000) - Set local benchmark for amount?
- Time pressure driving early completion of 3rd
stage
17
Issues for Midwifery Practice
- Dealing with midwives concern about potential
bleeding and time taken - Fish cant see water syndrome (Wagner, 2001)
- Need for exposure to physiological 3rd stage
- Need to remove time pressure (left alone for 1st
hour if possible) - Cease checking for nuchal cord (cordclamping.com,
2004) - Skill drills on physiological 3rd stage
18
Practice Recommendations
- Women should be encouraged to consider
physiological approach antenatally - Research evidence needs contextualising
- all studies in hospitals
- historical legacy re haemorrhage and time
pressure - medicalisation of childbirth
19
Practice Recommendations
- Midwives need reskilling in physiological care
- Physiological approach is the appropriate care
when labour is normal - Piecemeal approach not recommended
- If active chosen, risk/benefit of syntocinon 10
units v syntometrine need weighing
20
Questions
- How could you change the perception of the
physiology of 3rd stage where you work so that it
is viewed as normal for normal labour? - How would you ensure midwives are competent in
physiological third stage care? - What should be done about the current definition
of PPH? - Is there a need to review early clamping cutting
of the cord where you work?