Blood Pressure and Flow Overview - PowerPoint PPT Presentation
1 / 48
Title:
Blood Pressure and Flow Overview
Description:
Blood Pressure and Flow Overview emphasis on SYSTEMIC CIRCUIT Perfuses tissues with blood, Maintains flow to cappilaries Returns blood to heart Source of pressure – PowerPoint PPT presentation
Number of Views:215
Avg rating:3.0/5.0
Title: Blood Pressure and Flow Overview
1
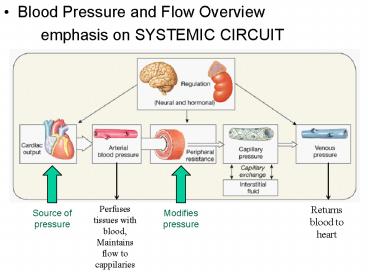
- Blood Pressure and Flow Overview
- emphasis on SYSTEMIC CIRCUIT
Perfuses tissues with blood, Maintains flow to
cappilaries
Returns blood to heart
Source of pressure
Modifies pressure
2
Fig. 13.26
Capillary bed
3
BLOOD FLOW
- Blood flows from high pressure areas to low
pressure areas - Blood flows through vascular system because of
these pressure differences - Arteries ? arterioles ? capillaries ? venules ?
veins
low pressure, no exchange
High pressure, no exchange
Low pressure, exchange occurs
4
Fig. 14.25
- As arteries and arterial branch and vessels
become more numerous, pressure decreases and
stays low until pumped through heart again.
5
Total Area -gtpressure-gtvelocity
Venous lower then arterial relate to relative
fractions in arterial v. venous components
6
Fig. 14.6
- Distribution of blood within vessels
- Average Blood Volume 5-6L
- Systemic Circuit 77 of all blood volume
- Venous system represents a reservoir of blood
that can be shunted to the arterial portion of
the system
7
About 5-6L of blood in average person Systemic
circuit 77 of all blood in vessel
8
- Systole
- Diastole
- MAP
- Elastic Rebound
9
Fig. 14.16
- Vessel-Pressure Patterns
- Pulsation and overall pressure decrease with
distance - Pulsation due to heart gone by capillaries
- Capillaries and veins are low pressure vessels
key for regulating BP
10
- Arterial Flow
- Systemic arterial pressure ranges from 120-35
mmHg - This pressure ensures blood flow through
capillaries where exchange happens - Vasoconstriction/Dilation
- 1. Regulates blood pressure
- Constriction/dilation of arterioles is most
important - Constriction increases Resistance ? increases BP
- Dilation decreases resistance ? decreases PB
- 2. Shunts blood (re-distributes it) to parrallel
circuits/other places
11
(No Transcript)
12
Figure 23.5
artery
arteriole
Capillary bed
venule
veins
13
(No Transcript)
14
- Capillary flow
- Low pressure
- 35mmHg-18mmHg
- Capillary beds
- interconnected networks of capillaries
- Local flow/vasomotion
- flow through capillaries is not constant, but is
regulated by precapillary sphincters (and
terminal arterioles) - Only 25 of capillaries experiences flow at any
moment (at rest) - Vessels are permeable
- Capillary exchange
15
- Capillary Exchange
- Diffusion/osmosis (due to concentration
gradients) - Between gaps in cells (ions and small organic
molecules) - Through transport proteins (ions)
- Through membrane lipids (lipid soluble
substances) - Filtration due to capillary hydrostatic pressure
(i.e., blood pressure in capillaries) 35-18mmHg - Primarily at arterial end of capillary drives net
filtration out of vessels ( 35 mmHg) - Osmotic pressure (colloid osmotic
pressure/oncotic pressure) - drives reabsorption of most fluid lost by
filtration - Minimized by reabsorption due to colloid osmotic
pressure - Primarily at venous end of capillary ( 18 mmHg)
- Active Transport
- Ion pumps
- Vessicular transport endocytosis brings
materials into one side of endothelium and
released to opposite site by exocytosis
16
(No Transcript)
17
Fig. 14.9
- If capillary hydrostatic pressure rises?
increased filtration and accumulation of fluid in
interstitial spaceedema - If blood volume declines due to bleeding,
capillary hydrostatic pressure/filtration
declines ? increased reabsorption (partially
compensating volume loss) - During dehydration colloid osmotic pressure
increases ? increased reabsorption (partially
compensating volume loss)
18
Fig. 13.37
- Net loss of fluid from capillaries results in
fluid flow - Plasma?
- interstitial space/fluid?
- lymph?
- plasma
- flushes interstitial fluid enhancing immune
system function - Keeps interstitial fluid and plasma in
communication - Increases distribution of materials especially
insoluble lipids that have difficulty crossing
capillary walls
19
Fig. 13.38
- Fluid lost from plasma enters lymph and is
eventually returned to plasma - No loss of plasma volume
- 3.6L/day transported as lymph
- Lost from capillaries
20
Fig. 14.10
21
- Venous Flow
- Low pressure 18mmHg 2mmHg
- Non-pulsile
- Venous reservoir
- Flows due to
- Small pressure gradient
- Muscle pump (skeletal muscle contraction
particularly the lower limbs) - Respiratory pump
- Contraction of diaphragm enhances venous return
22
- Muscle pump
- Constriction muscles compresses veins and
pressurizes blood - Valves ensure this blood moves towards heart
- Increased muscle use? increased venous return
23
- Regulation of Arterial Flow
- Extrinsic regulation
- SD-ANS
- Hormones
- Intrinsic (autoregulation) Regulation of local
flow - The state of vasoconstriction/dilation and blood
flow (and is due to the combined effects of both
autoregulation and extrinsic regulation
24
- Neuroendocrine regulation of BP and Blood Flow
Autoregulation of local flow
25
- Nervous System Regulation
- Vasoconstriction/Dilation
- Sympathetic Divison ANS (Vasomotor Centers of
Medulla) - Adrenergic Fibers (neurons)
- Most vessels (including skeletal muscle, see
below) - NE to alpha 1 receptors ? constriction
- Sympathetic Tonedefault state of partial
contraction - due to normal background SD activity
- Increased SD?
- Decreased SD?
- Cholinergic Fibers (neurons)
- Primarily Skeletal muscle
- Note skeletal muscle vessels have sypathetic tone
due to alpha andrenergic innervation - Ach to cholinergic receptors ? Dilation
- Skeletal muscle cells also have beta 2 adrenergic
receptors that are stimulated by epinephrine
released by adrenal medulla that promote
dilation.
26
Sympathetic tone, vasoconstriction and
vasodilation
Rate of SD signaling
27
- Autoregulation/Intrinsic Regulation of local
blood flow - local factors (including paracrine regulation) ?
changes in capillary bed flow - Due to constriction/dilation of precapillary
sphincters and arterioles - Factors
- decrease O2/increase CO2
- increase lactic acid/decrease pH
- NO increase
- K increase
- histamine release
- increase temperature
- increased stretch of vascular smooth muscle
- prostoglandins thromboxanes
promote dilation / increase flow
Myogenic mechanisms
promote constriction / decreased flow
released during tissue damage and during clotting
28
Fig. 14.24
- Constriction reduces flow to down stream
structures - Increases pressure and flow to upstream
structures.
Increased pressure and flow
Reduced flow
29
Regulation of BP
- Blood Pressure Influenced by
- CO
- Heart function
- Vascular Resistance
- more resistance increased BP
- Diameter of vessels
- dilation ? reduces resistance/BP
- Length of vessels
- Viscosity of blood
- Blood volume
- influenced by water balance (water uptake v.
water loss)
Changes in minutes
Changes in hours-days
30
Page 470
Primary factors influencing BP
- Vasoconstriction
- Vasodilation
- Blood Volume
31
- Blood Flow and Regulation of Systemic BP
- Blood must flow to tissues that need it
- BP must be sufficient to deliver blood adequately
- Perfussion
- lack of perfusion ? Ischemia/ischemic ?
infarction - Regulation of BP
- Intrinsic/Autoregulation of local flow
- Extrinsic Regulation
- Nervous systemsympathetic ANS
- Medulla vasomotor center
- Endocrine System/Hormonal regulation
- Mostly long term regulation of blood volume
- Hypothalamus?pituitary?Kidneys
32
Fig. 14.7
SV and CO
33
- Overview of cardiovascular regulation
34
- Baroreceptor reflex
- Baroreceptors (pressure) in carotid bodies and
aorta - Glossopharyngeal nerve (carotid bodies)
- Vagus nerve (aorta)
- Detect increases and decreases in pressure
- Send sensory impulses to medulla
- Cardiac center sends output to heartre CO
- SD (cardioaccelaratory) and PD (cardioinhibitory)
- Vasomotor center send output to vesselsre
constriction/dilation - SD
- BP maintained within normal range
35
Fig. 14.28
36
Fig. 14.28
Orthostatic/postural hypotension and barocrecptor
reflex
37
- Neural responses to changes in BP
?BP
?BP
VIS very important slide
38
- Endocrine/Hormonal Regulation of BP
- Mostly through regulation of blood volume
- But also vasoconstriction/dilation effects
- Hormones
- Antidiuretic Hormone (ADH, vasopressin)
- Angiotensin II
- Aldosterone
- Natriuretic Peptide
39
Fig. 14.11
- ADH
- Decreasing blood/plasma volume? increased solute
concentration (osmolality) - ADH release increases
- Increased fluid retention (less urine output)
- Increased water intake
- Blood volume stabilized/increased
40
Fig. 14.12
- Angiotensin II
- decreased Renal blood pressure
- Angiotensin II release
- Vasoconstriction
- Short term BP increase/stabilizer
- Aldosterone released
- Increased water retention (less urine output)
- Increased/stabilized blood volume
- Increased/stabilized BP
- ACE inhibitors for hypertension
41
- Response to ? blood vol./pressure
- Combined influence of
- ANSSD
- ADH
- Angiotensin II
- Aldosterone
Censored
Censored
42
Fig. 14.13
- Natriuretic Peptides and Increased BP
- High BP?Stretches atria
- Natriuretic peptide release
- Inhibits ADH release
- Increases water loss/urine output
- Blood volume decreases
- BP decreases
43
- Response to ? blood vol/pressure.
44
(No Transcript)
45
Changes in Systemic Blood Distribution With
Exercise
46
(No Transcript)
47
- Physiological (circulatory) Shock
- Inadequate perfusion (blood flow/BP)
- 3 fundamental causes
- Heart insufficient CO? BP inadequate
- Infarction, severe arrhythmias or valve damage
- Vessels widespread vasodilation ? BP inadequate
- Brain damage, endotoxins, or histamine (allergic
rxn) - Blood Volume too low ? BP inadequate
- Bleeding, burns, dehydration
48
Table 14.4
49
Table 14.5
50
Fig. 14.21