Evidence based decision making in pediatric physical therapy - PowerPoint PPT Presentation
1 / 29
Title:
Evidence based decision making in pediatric physical therapy
Description:
Evidence based decision making in pediatric physical therapy Pediatric physical therapy Infants ( under age2 years) Children ( from 2-12 years) adolescents ( from 13 ... – PowerPoint PPT presentation
Number of Views:226
Avg rating:3.0/5.0
Title: Evidence based decision making in pediatric physical therapy
1
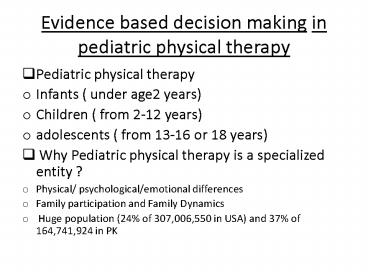
Evidence based decision making in pediatric
physical therapy
- Pediatric physical therapy
- Infants ( under age2 years)
- Children ( from 2-12 years)
- adolescents ( from 13-16 or 18 years)
- Why Pediatric physical therapy is a specialized
entity ? - Physical/ psychological/emotional differences
- Family participation and Family Dynamics
- Huge population (24 of 307,006,550 in USA) and
37 of 164,741,924 in PK
2
EBP VS. Non-Standard treatment
- Non-standard treatment
- not verified through the scientific study
- not published or included in peer-reviewed
journals - 90 treatment methods in physical therapy are
taken from professional education, continuing
education, and experience. - Turner and Whitfield, PTs use of EBP.
Physiotherapy Research International, 2(1), 1997
3
What is evidence based practice?Paradigm Shift
in 1992
- the conscientious, explicit and judicious use of
current best evidence in making decisions about
the care of individual patients - (Sackett et al, 1996)
- Barriers for achieving EBP
- Steps in achieving EBP
- Formulating a Question
- Finding Evidence
- Appraisal of evidence
- Translation of evidence to practice
- Evaluation of evidence
- the responsibility to deliver evidence based
treatment rests with all members of profession
not only with researchers
4
Finding Evidence
- Peer-reviewed journals Primary source of
evidence - sources
- Hard Copy libraries catalog
- Electronic databases ( e.g. MEDLINE, ERIC,
PsycINFO, PEDro, Cochrane, Hooked on evidence) - Expert Consensus/ expert opinions
- Secondary source of evidence ( e.g. practice
guideline, clinical pathway) e.g. C-Spine rule,
Ottawa Ankle rule - Appraisal of guidelines to research and
evaluation (AGREE) - Textbooks personal experiences are also
secondary sources of evidence
5
Appraisal of evidence
- All available evidence is not Diamond or Gold
- Important steps in appraisal ( primary source)
- Find out a relevant research that you think can
answer your question ( journal article/systematic
review, etc.) - Appraise Research design Quantitative Vs
Qualitative - Quantitative Research- Experimental Vs
non-experimental - Experimental research- true vs.
quasi-experimental or experimental research with
no control group - Internal Vs. External validity
- Efficacy (RCT) Vs. Effectiveness
(non-experimental)
6
Hierarchical Evidence Based Practice
7
Levels of Evidence
1 High quality meta-analysis (based on double blind) High quality RCT (double blind)
1 Good meta-analysis (based on single blind RCTs) Good RCT (single blind)
2 Poor quality meta-analysis (based on open studies) Poor RCT (open studies)
2 Cohort study
3 Outcomes, relationship, retrospective studies
4 Case report, expert opinion
8
Five-level system of evidence
- Used for experimental design ( for single
research) - Level I II for randomized control trial (RCT)
- Level III IV for Quasi-experimental design (
when there is no randomization) - Level V for quasi-experimental design ( when
there is no control group)
9
Grades of Recommendation for systematic reviews
- A systematic review is a comprehensive survey of
a topic in which all of the primary studies
relevant to topic have been systematically
identified, appraised and then summarized. - Grade A recommendation is for at least one level
I study - Grade B recommendation is for at least one level
II study - Grade C recommendation is for level III, IV or V
studies - Meta-analysis(studies that used inferential
statistics)
10
Translation of evidence to practice
- Evidence alone does not make decision, people
do - why in health care transfer of evidence is
practice is slow? - Patient/client their family perspectives
- Family dynamics
- Informed choices ( family voices, kid power)
- Cultural differences
- Financial resources
11
Clinical Reasoning and Decision Making
- Medical Model
- Person has a disease
- Treat the disease
- How are we going to cope with disease?
- Accepting person means we have change our
practice, and it will cost more. - Finally these persons are excluded
- Social model
- Person has an impairment
- What are the barriers?
- What are solutions to overcome barriers
- Diversity and cultural differences are accepted
- Finally these persons are included
12
Frameworks for Decision making
- Frameworks helps in clinical decision making (
diagnosis, intervention, prognosis, etc) - Nagi Model presented by Saad Nagi in 1965
- International Classification of Impairments,
disabilities, and Handicaps (ICIDH) published by
WHO in 1980 - International classification of Functioning,
disability (ICF) and Health by WHO in 2001.
13
Nagi Model
- Active Pathology Interruption or interference
of normal processes and efforts of the organism
to regain normal state. - Impairment Anatomical, physiological, mental,
or emotional abnormalities or loss. - Functional limitation Limitation in performance
at the level of the whole organism or person - Disability Limitation in performance of
socially defined roles and tasks within a
sociocultural physical environment
14
ICIDH
- Disease Intrinsic pathology or disorder
- Impairment Loss or abnormality of
psychological, physiological, or anatomical
structure or function at organ level - Disability Restriction or lack of ability to
perform an activity in a normal manner - Handicap Disadvantage resulting from impairment
or disability that limits or prevents
fulfillments of a normal role in community (
Depending age, sex, cultural factors)
15
ICF
- Body Functions and Structures Changes in body
functions (physiological) or structures
(anatomical). Change may be positive or negative(
impairment) - Activities Functioning at an individual level
- Participation Functioning at a societal level
- Activities and participation can be viewed in
terms of capacity and performance - Disability occurs when activities are limited or
participation in societal roles is restricted. - Example child with Hemiplegia
16
Patient/client Management Model
(adapted from the APTA Guide to PT practice)
17
Examination
- Physical therapists are educated and clinically
trained to perform a number of tests and measures
that can assess an impairment/problem - History ( General information core interview)
- General Information Age, Gender,
Race/ethnicity, Past medical/surgical history,
clinical tests - Core Interview History of present illness, pain
symptom assessment, medical treatment, current
level of fitness, review of systems - How to incorporate evidence in examination??
18
Patient/client Management Model cont..
- Evaluation
- Physical therapists can utilize data collected
during examination procedures to assess
impairment that may reflect current pathology,
and functional limitation, as well as the
propensity for future injury which may impact
quality of life, and mortality
- Diagnosis
- Physical therapists can utilize data collected
during examination procedures to provide a
physical therapy diagnosis including
impairments, and functional limitations - Examples of PT diagnosis
- Muscle weakness, muscle Imbalance, lack of
coordination
19
Patient/client Management Model cont..
- Prognosis
- Based on the outcomes measured during the
examination process, the PT can make statements
regarding potential benefits to be derived from
interventions that target impaired measurements,
as well as resultant or potential pathology, and
functional limitation.
- Interventions
- Physical therapists may provide
- coordination, communication, and documentation
- patient/client education
- direct intervention
20
outcomes
- What will be final outcomes?
- Minimize functional limitations
- Health promotion and wellness
- Optimization of patient/client satisfaction
- Prevention of disability
21
Evaluation of intervention/outcomes
- Case report ( non-experimental)
- Single subject design (experimental)
- ABA or withdrawal design
- A number of observations with no treatment (the A
or baseline sessions) are followed by a number of
observations with treatment (B). - If the treatment is successful, there should be
improvement on the Dependent variable in the B
sessions. - To show that the improvement is the effect of the
Independent variable and not maturation or
history, another no-treatment or A session is
given.
22
ABA or Withdrawal Design
A A A A B B B B A A A A
Baseline Phase 0 Baseline Phase 0 Baseline Phase 0 Baseline Phase 0 Treatment Phase Treatment Phase Treatment Phase Treatment Phase Withdrawal phase 0 Withdrawal phase 0 Withdrawal phase 0 Withdrawal phase 0
0 0 0 0 0 0 0 0 0 0 0 0
23
Physiotherapy program evaluation
- Overall monitoring of program effectiveness
- Evaluation of record keeping
- Monitoring of therapist adherence to program
policies - Monitoring of therapist interaction with client,
other health care provider, and third party
payers - Evaluation of client satisfaction and long-term
outcomes
24
Monitoring services within a database
- Multiple users
- Proper organization and storage of data
- Can easily be retrieved, updated and reorganized
- Requirement of Joint Commission on Accreditation
of Healthcare Organizations (JCAHO) Commission
on Accreditation of Rehabilitation Facilities (
CARF)
25
Formal Program Evaluation
- Mostly evaluated by a separate evaluating body
- Summative VS Formative evaluation
- Framework for program evaluation
- Does the method of service delivery represents
the best educational practices? - Is the intervention being implemented accurately
and consistently? - Is an attempt being made to verify the
effectiveness of intervention objectively? - Does the program carefully monitor patient
progress and demonstrate a sensitivity to points
in which changes in services need to be made? - Does a system exist for determining the adequacy
of patient progress and service delivery? - Is the program accomplishing its goals and
objectives? - Does the service delivery system meet the needs
and values of the community and clients it serves?
26
Circular versus Hierarchical EBP
- Hierarchical model based on pharmacology model of
therapy - Applied to other complex interventions
- Surgery
- Physiotherapy
- Occupational Therapy
- Complementary or Alternative Medicin
27
Circular EBP
- Multiplicity of methods
- Used in a complimentary fashion
- Each research method has strengths and weaknesses
- Achieve a result replicate with other methods
28
Circle of Methods
- Experimental methods that test specifically for
efficacy (upper half of the circle) have to be
complemented by observational, non-experimental
methods (lower half of the circle) that are more
descriptive in nature and describe real-life
effects and applicability.
29
- Questions
- Comments