Denied Claims: 6 Common Reasons and How to Solve Them - PowerPoint PPT Presentation
Title:
Denied Claims: 6 Common Reasons and How to Solve Them
Description:
Denied claims are a double-whammy: they negatively impact your surgical centre’s cash flow, and they also add to your overhead costs because it takes plenty of staff time to correct and resubmit the claims. – PowerPoint PPT presentation
Number of Views:1
Title: Denied Claims: 6 Common Reasons and How to Solve Them
1
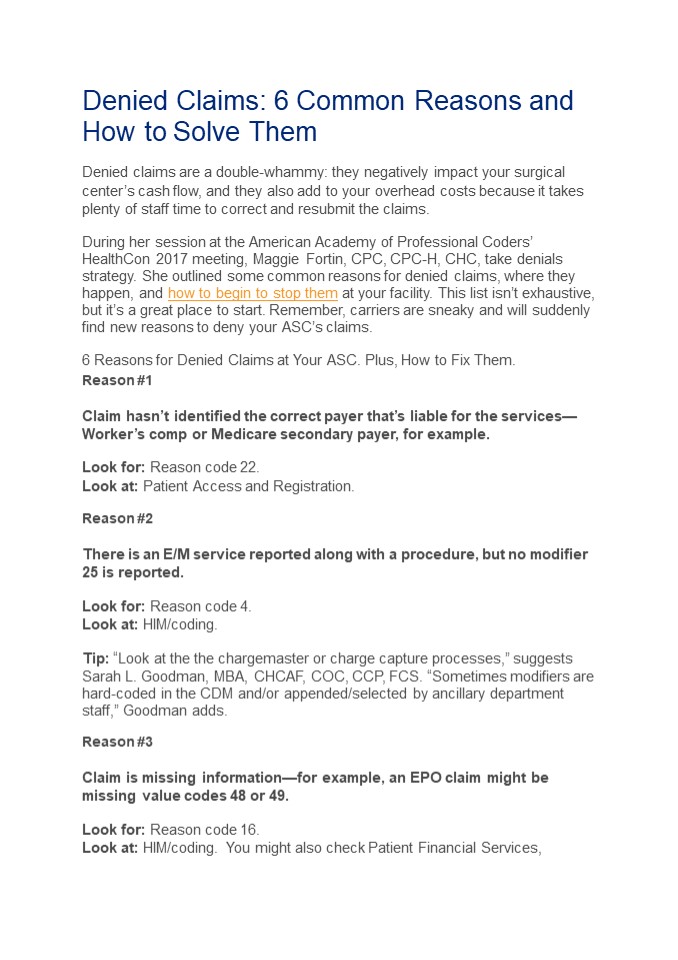
Denied Claims 6 Common Reasons and How to Solve
Them Denied claims are a double-whammy they
negatively impact your surgical centers cash
flow, and they also add to your overhead costs
because it takes plenty of staff time to correct
and resubmit the claims. During her session at
the American Academy of Professional Coders
HealthCon 2017 meeting, Maggie Fortin, CPC,
CPC-H, CHC, take denials strategy. She outlined
some common reasons for denied claims, where they
happen, and how to begin to stop them at your
facility. This list isnt exhaustive, but its a
great place to start. Remember, carriers are
sneaky and will suddenly find new reasons to deny
your ASCs claims. 6 Reasons for Denied Claims
at Your ASC. Plus, How to Fix Them. Reason
1 Claim hasnt identified the correct payer
thats liable for the servicesWorkers comp or
Medicare secondary payer, for example. Look for
Reason code 22. Look at Patient Access and
Registration. Reason 2 There is an E/M service
reported along with a procedure, but no modifier
25 is reported. Look for Reason code 4. Look
at HIM/coding. Tip Look at the the
chargemaster or charge capture processes,
suggests Sarah L. Goodman, MBA, CHCAF, COC, CCP,
FCS. Sometimes modifiers are hard-coded in the
CDM and/or appended/selected by ancillary
department staff, Goodman adds. Reason
3 Claim is missing informationfor example, an
EPO claim might be missing value codes 48 or
49. Look for Reason code 16. Look at
HIM/coding. You might also check Patient
Financial Services,
2
says Goodman. Sometimes missing codes may
originate from incorrect file maintenance. Reason
4 Claim has been denied because of another
service or procedure performed on the same
date. Look for Reason code 236. Look at
HIM/coding, NCCI edits. Look Out If you bill
two services together that shouldnt be due to
frequency, the payer wont just deny one and pay
the other. Both services will usually be denied,
and youll need to resubmit just one. Reason
5 Diagnosis reported did not meet LCD/NCD
guidelines. Look for Reason Code 50 Look at
Clinical documentation and/or HIM/coding.
Correcting diagnosis- related denials may mean
educating your physiciansanother place where
top-notch communication skills will come in
handy. Reason 6 Duplicate billing. Look for
Reason code 18. Look at Patient Financial
Services. Billing system may be failing to detect
duplicate claims.