Innate and Adaptive Immunity - PowerPoint PPT Presentation
1 / 31
Title:
Innate and Adaptive Immunity
Description:
CHEMOKINES are often first sign that host is infected ... Cutaneous immune system: keratinocytes, Langerhans cells and T-cells ... – PowerPoint PPT presentation
Number of Views:4435
Avg rating:3.0/5.0
Title: Innate and Adaptive Immunity
1
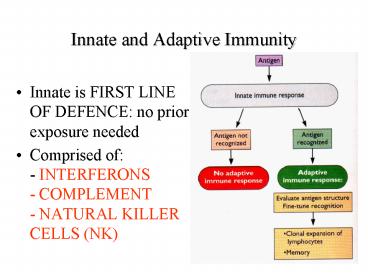
Innate and Adaptive Immunity
- Innate is FIRST LINE OF DEFENCE no prior
exposure needed - Comprised of- INTERFERONS- COMPLEMENT-
NATURAL KILLER CELLS (NK)
2
(No Transcript)
3
- INFLAMMATION
- initiated by CELL DAMAGE - activates COMPLEMENT,
MAST CELLS, etc. Symptoms are REDNESS, HEAT,
SWELLING, PAIN. - Neutrophil / macrophage chemotaxis into site
of inflammation increases response, results in
recruitment of T-cells, etc.
4
- CHEMOKINES are often first sign that host is
infected - Tend to act locally near cells that make them
- Participate in- CONTROL OF INFLAMMATION-
INDUCTION OF ANTIVIRAL STATE- REGULATION OF
ADAPTIVE IMMUNE RESPONSE - Invoke GLOBAL RESPONSES act on nervous system,
etc. Cause many classical signs of virus
infection
5
- Inflammatory cytokines IL-1, IL-6 and TNF act on
BRAIN and LIVER to produce symptoms and
ACUTE-PHASE PROTEINS - these have innate immune
capability eg activate complement, lymphocyte
production, etc.
6
- SPECIFICALLY ANTIVIRAL RESPONSE
- produced by infected cells - triggered by dsRNA,
some structural proteins, etc induction rapid,
and transient - secreted Ifn binds cell receptors 1 for, 1 for ?
- ?, ? induce antiviral state over 100 genes
induced leads to cell death by apoptosis if
prolonged - blocks cell proliferation, inc. NK cell activity,
etc. - induces dsRNA-activated Pkr, PO4ylates eIF2
- induces RNAse L and dsRNA-act. 2-5 oligoA
synthetase 2-5 oligoA act. RNAse L, degrades
mRNAs
7
Ifn-?/? and -? have different cell surface
receptors but sharecomponents Of the
Jak/Statsignal transduction pathway.Binding of
either type to thereceptors causes Tyr
PO4ylationof the different receptor-associated
kinases, and of thedifferent Stat proteins
associatedwith these. Ifn-?/? complex hasa
unique pathway activating p113both activate
p91/p84. These pathways then converge inthe
activation of Ifn-stimulatedresponse elements
(ISREs) theydiverge in that Ifn- ? can
inducegamma-activated site (GAS) genes
8
Viruses can block effects of interferon
9
- COMPLEMENT - a complex collection of serum
defence proteins that also amplifies immune
reactions. - 18 serum and roughly same no. membrane proteins
which act sequentially in a cascade - started by
ANTIGEN-C or Ab-C interaction. - Form MEMBRANE ATTACK COMPLEX to lyse cells - MOs,
viruses, RBCs, nucleated cells
10
- Classical pathway activated by C1 binding Ab-Ag
complex - Alternative pathway activated by C3b binding Ag
directly
11
Natural Killer Cells
- Large, granular lymphocytes, no Ag receptors
- Can constitute up to 30 of circulating
lymphocytes - Act early in infection, spontaneously kill
infected cells - Numbers expand quickly with viral infection,
decline with adaptive response - Lyse cells and secrete cytokines like Ifn-? and
Tnf-? - Bind cells via many receptors, including lectins
- Interaction with cells governed by ACTIVATION
signals (eg new CHO ligand) and NEGATIVE signal
(eg MHC class I protein).
12
(No Transcript)
13
Humoral and cellular response require activation
and proliferation of Th cells
14
Humoral response begins when Ag cross-links
several Ab receptors which are then endocytosed,
and is processed by proteolysis, complexed with
MHC class II molecules, and presented at the cell
surface. The Th cell then recognises this by
means of its T-cell receptor and secretes
cytokines to activate the cell to divide and
differentiate.
15
(No Transcript)
16
Cellular components of mucosa-associated
lymphoid tissue in gut.M cells and
intraepithelial lympho-cytes transfer antigen
from gut to lymphoid tissue in Peyers patches
Primary lymphatic systemshowing ducts and
nodesmobile dendritic cells meetcirculating
lymphocytes in nodes
17
Cutaneous immune systemkeratinocytes,
Langerhans cells and T-cellsKeratinocytes
secrete Tnf-?, IL-1 and IL-6 and havephagocytic
activity and have MHC-I and II and present Agto
T and B cells if stimulated by Ifn-?. Langerhans
cellsare migratory dendritic cells and have
MHC-I and II
18
B cells have 100 000-odd identical Ab monomers as
receptors. T cells have about 100 000 identical
receptors. T cells with CD4 receptors recognise
peptides bound toMHC class II proteins and are
generally Th cells. Cellswith CD8 receptors
recognise peptides bound to MHC-Iand generally
act as cytotoxic T cells.
19
Members of the Igsuperfamily of receptors
Antibody dimer of hetero-dimers heavy and
light chainsboth have variable regions
T-cell receptorheterodimer of an ? and a ?
chain or ?and ? chains, all withN-terminal V
domains.
20
CD4 and CD8 are bothglycosylated type I
membrane proteins, both of which have
cytoplasmicdomains which interactwith tyrosine
kinases, whichmeans they participate insignal
transduction events.Both have Ig-like
variabledomains. CD4 molecules are monomers and
bind MHC class II proteins via the 1sttwo
domains. CD8 proteinsare heterodimers linked
bydisulphide bridges. Theybind MHC class I
proteins.
21
Both are heterodimers,but MHC-I ? chain has 3
domains and ?2 only 1 while MHC-II ? and ? each
have 2. MHC class I are found on nearly all
nucleated cells, but at highest concentration on
lymphocytes (500 000 vs 100/cell on liver cells).
MHC-II are found only on specialist APCs. There
are 3 loci for each type (A, B, C
for I, DR, DP and DQ for II), but many alleles,
meaning individual responses will differ
considerably. Ifns stimulate MHC-I production.
22
(No Transcript)
23
(No Transcript)
24
Full activation of Th cells in many cases
requires interaction of othersurface proteins
and co-stimulators on the APC and T-cell as well
as the TCR and MHC class II proteins. Activated
Th cells make IL-2and IL-2 receptor resulting in
autostimulation. CTLs (CD8 T-cells)require at
least 3 additional reactions, including TCR/MHC-I
binding, binding of other surface proteins on
the CTL with the target cell, and binding of
cytokines produced by Th1 cells nearby.
25
Immature T-cells can differentiate into Th1 or
Th2 classes, distinguished by the cytokines they
produce. They have distinct functions and
respond to Ag stimulation with a transient burst
of cytokine stimulation that differentially
influences the activation and proliferation of
other immune cells. Th1 cells promote
maturation of CTLs and arm APCs. IL-12
induces immature Th cells to mature to
Th1s IL-4 prompts -gt Th2. These
promote B cell maturation. Th1 Induce
IgG2a, which activates C1 and binds
macrophages
Th2 stimulate IgG4 and IgE, which do not. Th1
Th2 see-saw
26
The first Abs expressed by a VIRGIN B-CELL are
MEMBRANERECEPTOR IgM/IgD. Binding and
cross-linking of receptors byan antigen triggers
a signal transduction cascade, which
whenreinforced by Th2-produced cytokines and
growth factors secretedby macrophages, result in
cell proliferation and differentiation
andincreased soluble Ab production, then
CLASS-SWITCHING anddifferentiation to memory and
plasma cells. Memory cells last formonths to
years plasma cells last only a week or so.
27
How antibodies can interfere in virus infection
normal cell entry isshown at left what can
happen with antibodies at right. Ab can (1)
aggregate (2) neutralise (3) stabilise (4)
change virion structure(5) potentially enter
cell and interfere within
28
IgA secretory antibodies play a keyrole in
antiviral defence at mucosalsurfacesPlasma
cells secrete polymeric IgA(pIgA) that binds a
receptor on theinner side of an epithelial cell.
ThepIgA is endocytosed and deliveredinto
vesicles targetted to the outerside of the cell
(TRANSCYTOSIS).pIgA is then released by
proteolysisof the receptor pIgR by a
surfaceprotease.The IgA can bind to Ag at any
stageof the process it can take Ag into
thecell and across into the lumen it canblock
virus attachment in the lumenit can bind
internally and block virusmaturation / release
29
(No Transcript)
30
(No Transcript)
31
(No Transcript)