Urinary System - PowerPoint PPT Presentation
Title:
Urinary System
Description:
... Nephron 26-* Other Hormones Atrial natriuretic hormone Produced by right atrium of heart when blood volume increases stretching ... Facilitated diffusion Active ... – PowerPoint PPT presentation
Number of Views:232
Avg rating:3.0/5.0
Title: Urinary System
1
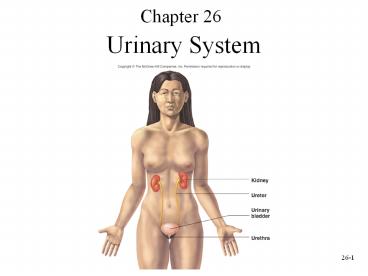
Chapter 26
- Urinary System
2
Urinary System Functions
- Filtering of blood involves three processes-
filtration, reabsorption, secretion. - Regulation of
- Blood volume
- Concentration of blood solutes Na, Cl-, K,
Ca2, HPO4-2 - pH of extracellular fluid secrete H
- Blood cell synthesis (kidneys secrete
hormone,erythropoietin) - Synthesis of vitamin D
3
Urinary System Anatomy
4
Location and External Anatomyof Kidneys
- External Anatomy
- Renal capsule fibrous connective tissue.
Surrounds each kidney - Perirenal fat
- Engulfs renal capsule and acts as cushioning
- Renal fascia thin layer loose connective tissue
- Anchors kidneys and surrounding adipose to
abdominal wall - Hilum
- Renal artery and nerves enter and renal vein and
ureter exit kidneys - Opens into renal sinus (cavity filled with fat
and loose connective tissue)
- Location
- Lie behind peritoneum (retroperitoneal) on
posterior abdominal wall on either side of
vertebral column - Lumbar vertebrae and rib cage partially protect
- Right kidney slightly lower than left
5
Internal Anatomy of Kidneys
- Cortex outer area
- Renal columns part of cortical tissue that
extends into medulla - Medulla inner area surrounds renal sinus
- Renal pyramids cone-shaped. Base is boundary
between cortex and medulla. Apex of pyramid is
renal papilla, points toward sinus. - Calyces
- Minor papillae extend into funnel of minor calyx
- Major converge to form pelvis
- Pelvis enlarged chamber formed by major calyces
- Ureter exits at the hilum connects to urinary
bladder
6
The Nephron
- Functional and histological unit of the kidney
- Parts of the nephron Bowmans capsule, proximal
tubule, loop of Henle (nephronic loop), distal
tubule - Urine continues from the nephron to collecting
ducts, papillary ducts, minor calyses, major
calyses, and the renal pelvis - Collecting ducts, parts of the loops of Henle,
and papillary ducts are in the renal medulla
7
Types of Nephrons
- Juxtamedullary nephrons. Renal corpuscle near the
cortical medullary border. Loops of Henle extend
deep into the medulla. - Cortical nephrons. Renal corpuscle nearer to the
periphery of the cortex. Loops of Henle do not
extend deep into the medulla. - Renal corpuscle. Bowmans capsule plus a
capillary bed called the glomerulus.
8
Renal Corpuscle
- Bowmans capsule outer parietal (simple squamous
epithelium) and visceral (cells called podocytes)
layers. - Glomerulus network of capillaries. Blood enters
through afferent arteriole, exits through
efferent arteriole.
9
Bowmans Capsule
- Parietal layer outer. Simple squamous epithelium
that becomes cube-shaped where Bowmans capsule
ends and proximal tubule begins - Visceral layer inner. Specialized podocytes that
wrap around the glomerular capillaries
10
Filtration Membrane
- Fenestrae window-like openings in the
endothelial cells of the glomerular capillaries. - Filtrations slits gaps between the cell
processes of the podocytes. Basement membrane
sandwiched between the endothelial cells of the
glomerular capillaries and the podocytes. - Filtration membrane capillary endothelium,
basement membrane and podocytes. First stage of
urine formation occurs here when fluid from blood
in capillaries moves across filtration membrane
into the lumen inside Bowmans capsule.
11
Circulation in the Glomerulus
- Afferent arteriole supplies blood to glomerulus
- Efferent arteriole drains glomerulus
- Both vessels have a layer of smooth muscle
- Juxtaglomerular apparatus sight of renin
production - Juxtaglomerular cells- ring of smooth muscle in
the afferent arteriole where the latter enters
Bowmans capsule - Macula densa- Specialized tubule cells of the
distal tubule. The distal tubule lies between the
afferent and efferent arterioles.
12
Histology of the Nephron
- Proximal tubule simple cuboidal epithelium with
many microvilli - Loops of Henle
- Descending limb first part similar to proximal
tubule. Latter part simple squamous epithelium
and thinner - Ascending limb first part simple squamous
epithelium and thin, distal part thicker and
simple cuboidal - Distal tubule shorter than proximal tubule.
Simple cuboidal, but smaller cells and very few
microvilli - Collecting ducts form where many distal tubules
come together. Larger in diameter, simple
cuboidal epithelium. Form medullary rays and lead
to papillary ducts
13
Circulation Through the Kidney
- Arterial supply
- Renal arteries branch from abdominal aorta
- Segmental arteries branch from renal
- Interlobar arteries ascend within renal columns
toward cortex - Arcuate arteries branch and arch overthe base of
the pyramids - Interlobular arteries project into cortex and
give rise to afferent arterioles
14
Circulation Through the Kidney
- The part of the circulation involved with urine
formation - Afferent arterioles supplyblood to glomerulus
- Glomerulus
- Efferent arterioles exit therenal corpuscle
- Peritubular capillaries form a plexus around the
proximal and distal tubules - Vasa recta (loop of henle) specialized parts of
peritubular capillaries that course into medulla
along with loops of Henle, then back toward cortex
15
Circulation Through the Kidney
- Venous drainage
- Peritubular capillaries (PCT) drain into
interlobular veins and lead to - Arcuate veins
- Interlobar veins
- Renal veins
16
Urine Formation
- Nephrons considered functional units of the
kidney smallest structural component capable of
producing urine
17
Filtration
- Movement of fluid, derived from blood flowing
through the glomerulus, across filtration
membrane - Filtrate water, small molecules, ions that can
pass through membrane (large molecules blood
cells protein-------do not pass) - Pressure difference forces filtrate across
filtration membrane - Renal fraction part of total cardiac output that
passes through the kidneys. Varies from 12-30
averages 21 - Renal blood flow rate 1176 mL/min
- Renal plasma flow rate renal blood flow rate X
fraction of blood that is plasma 650 mL/min
(1176 ml/min x 0.55 646.8 ml plasma/min) - Filtration fraction part of plasma flowing
through the kidney that is filtered into lumen of
Bowmans capsules average 19 - ( 650 ml plasma/min x 0.19 123.5 ml
plasma/min---------125 ml/min of filtrate) - Glomerular filtration rate (GFR) amount of
filtrate produced each minute. 180 L/day - Average urine production/day 1-2 L. Most of
filtrate must be reabsorbed
18
(No Transcript)
19
Filtration
- Filtration membrane filtration barrier. It
prevents blood cells and proteins from entering
lumen of Bowmans capsule, but is many times more
permeable than a typical capillary - Fenestrated endothelium, basement membrane and
pores formed by podocytes - Some albumin and small hormonal proteins enter
the filtrate, but these are reabsorbed and
metabolized by the cells of the proximal tubule.
Very little protein normally found in urine - Filtration pressure pressure gradient
responsible for filtration forces fluid from
glomerular capillary across membrane into lumen
of Bowmans capsules - Forces that affect movement of fluid into or out
of the lumen of Bowmans capsule - Glomerular capillary pressure (GCP) blood
pressure inside capillary tends to move fluid out
of capillary into Bowmans capsule - Capsule pressure (CP) pressure of filtrate
already in the lumen - Blood colloid osmotic pressure (BCOP) osmotic
pressure caused by proteins in blood. Favors
fluid movement into the capillary from the lumen.
BCOP greater at end of glomerular capillary than
at beginning because of fluid leaving capillary
and entering lumen - Filtration pressure (10 mm Hg) GCP (50 mm Hg)
CP (10 mm Hg) BCOP (30 mm Hg)
20
Filtration Pressure
21
Filtration
- Colloid osmotic pressure in Bowmans capsule
normally close to zero. During diseases like
glomerular nephritis, proteins enter the filtrate
and filtrate exerts an osmotic pressure,
increasing volume of filtrate - Filtrate is forced across filtration membrane
fluid moves into peritubular capillaries from
interstitial fluid - Changes in afferent and efferent arteriole
diameter alter filtration pressure - Dilation of afferent arterioles/constriction
efferent arterioles increases glomerular
capillary pressure, increasing filtration
pressure and thus glomerular filtration
22
Autoregulation and Sympathetic Stimulation
- Autoregulation
- Involves changes in degree of constriction in
afferent arterioles - As systemic BP increases, afferent arterioles
constrict and prevent increase in renal blood
flow (opposite also occurs) - Increased rate of blood flow of filtrate past
cells of macula densa signal sent to
juxtaglomerular apparatus, afferent arteriole
constricts - Sympathetic stimulation norepinephrine
- Constricts small arteries and afferent arterioles
- Decreases renal blood flow and thus filtrate
formation - During shock or intense exercise intense
sympathetic stimulation, rate of filtrate
formation drops to a few ml - Note Glomerular filtration rate is relatively
constant as B.P. changes between 90 180
mmHg.
23
Tubular Reabsorption Overview
- Tubular reabsorption occurs as filtrate flows
through the lumens of proximal tubule, loop of
Henle, distal tubule, and collecting ducts - Results because of
- Diffusion
- Facilitated diffusion
- Active transport
- Symport
- Osmosis
- Substances transported to interstitial fluid and
reabsorbed into peritubular capillaries
inorganic salts, organic molecules, 99 of
filtrate volume. These substances return to
general circulation through venous system
24
Reabsorption in Proximal Convoluted Tubule
- Substances pass through cells of tubule wall.
Each cell has - Apical surface surface that faces filtrate.
Apical membrane - Basal surface faces interstitial fluid. Basal
membrane - Lateral surfaces surfaces between cells
- Active transport of Na across the basal membrane
from cytoplasm to interstitial fluid linked to
reabsorption of most solutes
- Because of active transport, the concentration of
Na is low inside the cell and Na moves into
nephron cell from filtrate through the apical
membrane. Other substances moved by symport from
the filtrate into the nephron cell are substances
that should be retained by the body - Substances transported
- Through apical membrane Na, Cl-, glucose, amino
acids, and water. - Through basal membrane Na, K,
- Cl-, glucose, amino acids, water
25
Reabsorption in Proximal Convoluted Tubule
- Number of carrier molecules limits rate of
transport - In diabetes mellitus
- Concentration of glucose in filtrate exceeds rate
of transport - High concentration of glucose in plasma (and thus
in filtrate) reflected in glucose in the urine - Diffusion between cells from lumen of nephron
into interstitial fluid - Depends on rate of transport of some solutes
through the cells of the tubule - K, Ca2, and Mg2
- Filtrate volume reduced by 65 due to osmosis of
water
26
Reabsorption in Loop of Henle
- Loop of Henle descends into medulla interstitial
fluid is high in solutes. - Descending thin segment is highly permeable to
water and moderately permeable to urea, sodium,
most other ions (passive). - Water moves out of nephron, solutes in. Volume of
filtrate reduced by another 15. - Ascending thin segment is not permeable to water,
but is permeable to solutes. Solutes diffuse out
of the tubule and into the more dilute
interstitial fluid as the ascending limb projects
toward the cortex. Solutes diffuse into the
descending vasa recta.
27
Reabsorption in Loop of Henle
- The wall of the ascending limb of the loop of
Henle is not permeable to water. Na moves across
the wall of the basal membrane by active
transport, establishing a concentration gradient
for Na. K and Cl- are symported with Na across
the apical membrane and ions pass by facilitated
diffusion across the basal cell membrane of the
tubule cells. - At the end of the loop of Henle, inside of
nephron concentration of solutes is 100 mOsm/kg
(milli-osmole per kilogram). Interstitial fluid
in the cortex is 300mOsm/kg. Filtrate within DCT
is much more dilute than the interstitial fluid
which surrounds it.
28
Reabsorption in Distal Convoluted Tubule and
Collecting Duct
- Active transport of Na out of tubule cells into
interstitial fluid with cotransport of Cl- - Na moves from filtrate into tubule cells due to
concentration gradient - Collecting ducts extend from cortex (interstitial
fluid 300 mOsm/kg) through medulla (interstitial
fluid very high) - Water moves by osmosis from distal tubule and
collecting duct into more concentrated
interstitial fluid - Permeability of wall of distal tubule and
collecting ducts have variable permeability to
water - Urine can vary in concentration from low volume
of high concentration to high volume of low
concentration
29
Changes in Concentration of Solutes in the Nephron
- Urea enters glomerular filtrate.
- As volume of filtrate decreases (approx. 99 H2O
is reabsorbed), concentration of urea increases - Walls of nephron not very permeable to urea only
40-60 passively reabsorbed - Urate ions, creatinine, sulfates, phosphates,
nitrates partially reabsorbed - Concentration is high in urine
- Toxic substances and are eliminated
30
Tubular Secretion
- Moves metabolic by-products, drugs, molecules not
normally produced by the body into tubule of
nephron - Active or passive
- Ammonia produced by epithelial cells of nephron
from deamination of amino acids. Diffuses into
lumen - H, K, penicillin, and substances such as
para-aminohippuric acid (PAH) actively secreted
into nephron
31
Secretion of Hydrogen and Potassium
- Hydrogen ions secreted into filtrate by
countertransport in proximal tubule - H either diffuse from peritubular capillaries
into interstitial fluid and then into epithelial
cells of tubule or derived from reaction between
carbon dioxide and water in cells of tubule. - Na and HCO3- cotransported across basal membrane
into interstitial fluid, then diffuse into
peritubular capillaries
32
Secretion of Hydrogen and Potassium
- H and K secreted into filtrate by
countertransport in distal tubule. Na and K
move by active transport across the basal
membrane. Na and HCO3- cotransported across
basal membrane into interstitial fluid, then
diffuse into peritubular capillaries
33
Urine Production
- In ascending limb of loop of Henle
- Na, Cl-, K transported out of filtrate
- Water remains
- In distal convoluted tubules and collecting ducts
- Water movement out regulated by ADH
- If absent, water not reabsorbed and dilute urine
produced - If ADH present, water moves out, concentrated
urine produced
- In Proximal convoluted tubules
- Na and other substances removed
- Water follows passively
- Filtrate volume reduced
- In descending limb of loop of Henle
- Water exits passively, solute enters
- Filtrate volume reduced 15
34
Urine Concentration Mechanism
- When large volume of water consumed
- Eliminate excess without losing large amounts of
electrolytes - Response is that kidneys produce large volume of
dilute urine - When drinking water not available
- Kidneys produce small volume of concentrated
urine - Removes waste and prevents rapid dehydration
- Mechanisms that create urine of variable
concentration - Maintenance of high concentration of solutes in
medulla - Countercurrent functions of loops of Henle
- Control of permeability of distal nephron to
water
35
Medullary Concentration Gradient
- In order to concentrate urine (and prevent a
large volume of water from being lost), the
kidney must maintain a high concentration of
solutes in the medulla - Interstitial fluid concentration (mOsm/kg) is 300
in the cortical region and gradually increases to
1200 at the tip of the pyramids in the medulla - Maintenance of this gradient depends upon
- Functions of loops of Henle
- Vasa recta flowing countercurrent to filtrate in
loops of Henle - Distribution and recycling of urea
36
Creating/Maintaining High Solute Concentration in
Medulla
- Active transport of Na and cotransport of ions
such as K and Cl- and other ions out of the
thick portion of ascending limb into interstitial
fluid - Impermeability of thin and thick parts of
ascending limb of loop of Henle to water - Vasa recta remove excess water and solutes that
enter the medulla without destroying the high
concentration of solutes in interstitial fluid of
medulla - Active transport of ions from collecting ducts
into interstitial fluid of medulla - Passive diffusion of urea from collecting ducts
into interstitial fluid of medulla,
impermeability of the ascending limb and
permeability of the descending limb of the loops
of Henle to urea
37
Loops of Henle
- Juxtamedullary nephrons long loops.
- Walls of descending limbs permeable to water,
water moves out into interstitial fluid - Walls of ascending limb impermeable to water
- Solute diffuses out of thin segment of ascending
limb as it passes though progressively less
concentrated interstitial fluid - Na, K and Cl- actively transported out of
ascending limb into interstitial fluid - Thus, water enters interstitial fluid from
descending limbs and solutes enter interstitial
fluid from ascending limbs
38
Vasa Recta
- Countercurrent systems that remove excess water
and solutes from medulla parallel tubes in which
fluid flows, but in opposite directions - Blood flows through vasa recta to the medulla,
vessels turn near tip of renal pyramid, then
blood flows in opposite direction - Walls are permeable to water and to solutes as
blood flows toward medulla, water moves out,
solutes diffuse in. As blood flows back toward
cortex, water moves into vasa recta, some solutes
diffuse out - Diffusion is such that slightly more water and
slightly more solute are carried from the medulla
by the vasa recta than enter it
39
- Loops of Henle and vasa recta function together
to maintain a high concentration of solutes in
the interstitial fluids of the medulla and to
carry away the water and solutes that enter the
medulla from the loops of Henle and collecting
ducts - Water moves out of descending limb and enters
vasa recta - Solutes diffuse out of ascending thin segment and
enter vasa recta, but water does not - Solutes transported out of thick segment of
ascending enter the vasa recta - Excess water and solutes carried away from
medulla without reducing high concentration of
solutes - Concentration of filtrate reduced to 100 mOsm/kg
by the time it reaches distal tubule
40
- Water and solutes move out of the collecting duct
into the vasa recta
41
Urea
- Responsible for large part of high osmolality in
medulla - Descending limbs of loops of Henle permeable to
urea urea diffuses into interstitial fluid - Ascending limbs and distal tubules impermeable to
urea - Collecting ducts permeable to urea some diffuses
out into interstitial fluid - Urea flows in a cycle maintaining high urea
concentration in medulla
42
Urine Concentrating Mechanisms
43
Renin/Angiotensin/Aldosterone
44
ADH and the Nephron
45
ADH and the Nephron
46
Other Hormones
- Atrial natriuretic hormone
- Produced by right atrium of heart when blood
volume increases stretching cells - Inhibits Na reabsorption
- Inhibits ADH production
- Increases volume of urine produced
- Venous return is lowered, volume in right atrium
decreases - Prostaglandins and kinins produced in kidney.
Role unclear
47
Clearance and Tubular Maximum
- Plasma clearance calculated using substances
like inulin - Volume of plasma cleared of a specific substance
each minute - Used to estimate GFR
- Used to calculate renal plasma flow. Calculated
using substances like PAH - Used to determine which drugs or other substances
excreted by kidney - Tubular load
- Total amount of substance that passes through
filtration membrane into nephrons each minute
48
Tubular Maximum
- Maximum rate at which a substance can be actively
absorbed - Each substance has its own tubular maximum
- Normally, glucose concentration in the plasma
(and thus filtrate) is lower than the tubular
maximum and all of it is reabsorbed none of it
is found in the urine - In diabetes mellitus tubular load exceeds tubular
maximum and glucose appears in urine. Urine
volume increases because glucose in filtrate
increases osmolality of filtrate reducing the
effectiveness of water reabsorption
49
Urine Movement
- Hydrostatic pressure forces urine through nephron
- Peristalsis moves urine through ureters from
region of renal pelvis to urinary bladder. Occur
from once every few seconds to once every 2-3
minutes - Parasympathetic stimulation increase frequency
- Sympathetic stimulation decrease frequency
- Ureters enter bladder obliquely through trigone.
Pressure in bladder compresses ureter and
prevents backflow
50
Anatomy and Histology of Ureters and Bladder
- Ureters bring urine from renal pelvis to urinary
bladder. Lined by transitional epithelium - Urinary bladder hollow muscular container. In
pelvic cavity posterior to symphysis pubis. Lined
with transitional epithelium muscle part of wall
is detrusor
- Trigone interior of urinary bladder. Triangular
area between the entry of the two ureters and the
exit of the urethra. Area expands less than rest
of bladder during filling
51
Anatomy and Histology of Urethra
- Male extends from the inferior part of the
urinary bladder through the penis - Female shorter opens into vestibule anterior to
vaginal opening - Internal urinary sphincter in males, elastic
connective tissue and smooth muscle keep semen
from entering urinary bladder during ejaculation - External urinary sphincter skeletal muscle
surrounds urethra as it extends through pelvic
floor. Acts as a valve
52
Micturition Reflex
53
Effects of Aging
- Gradual decrease in size of kidneys, but only
one-third of one kidney necessary for homeostasis - Amount of blood flowing through gradually
decreases - Number of glomeruli decrease and ability to
secrete and reabsorb decreases - Ability to concentrate urine declines and kidney
becomes less responsive to ADH and aldosterone - Reduced ability to participate in vitamin D
synthesis contributing to Ca2 deficiency,
osteoporosis, and bone fractures