Leukocytes 4-10 000/mm3 Differential count: neutrophils 60- 70%, eosinophils 2-4% basophils - up to 1% ly: 20 – 30%, mono 3-8% - PowerPoint PPT Presentation
1 / 46
Title:
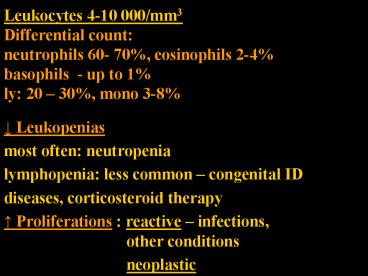
Leukocytes 4-10 000/mm3 Differential count: neutrophils 60- 70%, eosinophils 2-4% basophils - up to 1% ly: 20 – 30%, mono 3-8%
Description:
Leukocytes 4-10 000/mm3 Differential count: neutrophils 60- 70%, eosinophils 2-4% basophils - up to 1% ly: 20 30%, mono 3-8% Leukopenias most often: neutropenia – PowerPoint PPT presentation
Number of Views:248
Avg rating:3.0/5.0
Title: Leukocytes 4-10 000/mm3 Differential count: neutrophils 60- 70%, eosinophils 2-4% basophils - up to 1% ly: 20 – 30%, mono 3-8%
1
Leukocytes 4-10 000/mm3Differential
countneutrophils 60- 70, eosinophils
2-4basophils - up to 1ly 20 30, mono 3-8
- ? Leukopenias
- most often neutropenia
- lymphopenia less common congenital ID
- diseases, corticosteroid therapy
- ? Proliferations reactive infections,
other conditions - neoplastic
2
- NEOPLASTIC PROLIFERATIONS
- OF WHITE CELLS
- myeloid
- from the hematopoietic stem cells giving rise to
cells of myeloid lineage thrombocytic,
granulocytic, erythroid - Acute myelogenous (myeloid) leukaemias
- Myelodysplastic syndromes
- Chronic myeloproliferative disorders
- B. lymphoid - tumors of lymphocytes, lymphomas
and leukaemia - Hodgkin lymphoma versus non-Hodgkin lymphomas
- B- versus T- cell lymphomas
- precursor cells (B or T or NK) lymphoblastic
- versus mature cells B or T (or NK)
- C. histiocytic proliferative lesions of
histiocytes - Langerhans histiocytosis
3
Myelodysplastic syndrome
- Bone marrow(BM)
- Hyper /normocellular
- Dysplastic architecture, cytology
- Ineffective bone marrow failure
- Peripheral blood (PB) - pancytopenia
- Blood cells few and pathological
- (size, shape, function)
4
Myelodysplastic syndrome
- clonal disorders of stem cells
- defects of maturation in the BM - ineffective
hematopoiesis (progressive failure of BM
function) - cells in the PB decreased numbers
pancytopenia defective in function,
pathological shapes
- BM hypercellular,
- but dysplastic pathological forms, architecture
- blasts may be increased
- (but less than 20, threshold AML versus MDS)
5
Myelodysplastic syndrome
- Clinical symptoms and complications ???
6
Myelodysplastic syndrome
- Clinical symptoms and complications
- Anemia
- Thrombocytopenia - bleeding
- Leukopenia infection
- (Splenomegaly -)
- Asymptomatic one half
7
Myelodysplastic syndrome
- primary de novo - old people over 60
- secondary therapy related toxic exposure -
worse prognosis, more prone to AML
8
Myelodysplastic syndrome
- Subcategories
- Refractory anemia unilineage dysplasia
- RA with ringed sideroblasts the nucleus
encircled by siderotic granules - RA with multilineage dysplasia
- RA with excess blasts more than 5, less than
20 - MDS unclassifiable
- MDS assoc. with isolated del. (5q) chromosome
9
Chronic myeloproliferative diseases
10
Chronic myeloproliferative diseases
- Clonal disorders
- Adults
- 1. Chronic myeloid leukemia
- 2. Polycythemia vera
- 3. Essential thrombocytemia
- 4. Chronic osteomyelofibrosis
11
Chronic myeloproliferative diseases
- Common principles
- 1. Bone marrow stem cell genetic abnormalities,
- neoplastic proliferation of one or more (all) BM
myeloid series (red, white, megakaryocytes) - disorder of an individual series more pronounced
in each of the categories - 2. Peripheral blood increased numbers of cells
relatively normal maturation - 3. Splenomegaly, hepatomegaly
- sequestration of excess blood cells,
extramedullary hematopoiesis, leukaemic
infiltration
12
Chronic myeloproliferative diseasescommon
features
- phases of the disease in time
- 1. onset insidious
- proliferative phase,
- 2. progression - spent phase -
osteomyelofibrosis - - blast phase
- all can (do not have to) progress to AL CML does
it invariably)
13
Chronic myelogenous leukaemia (CML)
- t(9 22) Philadelphia chromosome, bcr-abl gene
pluripotent stem cell defect - abnormal fusion protein - increased tyrosine
kinase activity - most striking proliferation of G
- increased cellularity
- maturation retained (no hiatus leukaemicus)
- hematopoiesis also extramedullary splenomegaly
(hepatomegaly) - PB leukocytosis exceeds even 100 000/ mm3
14
CML
PB no hiatus leukaemicus mature neutrophils,
some metamyelocytes, and a myelocyte.
15
Chronic myelogenous leukaemia (CML)
- Phases
- 1. chronic aver. 3 ys
- 2. accelerated gradual failure of response to
treatment, increasing anemia and
thrombocytopenia, basophilia - 3. blast crisis after accelerated phase or
without the acceler. phase - Blast crisis acute leukaemia - 70 myeloid,
30 lymphoblastic
16
Chronic myeloid leukaemia
17
Chronic myeloid leukaemia
uric acid deposition
18
JAK2 mutation
- In one half
- of
- Polycythemia vera
- Essential thrombocythemia
- Chronic myelofibrosis
19
Polycythaemia veramorbus Vaquez
- increased proliferation of all three series
- most striking red cells
- hypercellular BM
- PB HTC 60, Hb over 180g/l
- For the diagnosis exclude secondary polycythemia
20
Polycythaemia vera
- increased RC mass - symptoms
- hypervolemia, blood stasis (mostly venous),
cyanosis stagnation and deoxygenation of blood - hypertension, thromboses, bleeding abnormal
blood flow, abnormalities of PLT - granulopoiesis may be elevated
- plt elevated functional abnormalities
- SPENT PHASE myelofibrosis
- (20/10 ys)
21
Polycythemia vera. Plethora.
22
Polycythemia vera. Plethora.
23
Polycythemia vera distension of retinal vessels
24
Polycythemia vera Gout - right great toe
25
Gouty tophi
26
Polycythemia vera, spent phase, advanced marrow
myelofibrosis. Massive splenomegaly (3020 gm
normal 150 to 200 gm) largely owing to
extramedullary hematopoiesis
27
Essential thrombocythaemia
- the least common CMPD
- PLT exceed 600 000 /mm3
- BM increased cellularity,
- megakaryocytes abnormal,
- often large
- PB PLT often large
- Symptoms
- thrombosis and hemorrhage abnormalities of
quantity and quality of PLT - rel. indolent
Giant platelets
28
Essential thrombocythaemia
haemorrhages
29
Essential thrombocythaemia
thrombosis, gangrene
30
Chronic idiopathic myelofibrosis
- Myelofibrosis with myeloid metaplasia
- Agnogenic myeloid metaplasia
31
Chronic idiopathic myelofibrosis
- abnormal neoplastic megakaryocytes release
fibrogenic factors PDGF and TGFa - stimulate fibroblasts to proliferation
- early BM hypercellular, minimal fibrosis
- progression BM hypocellular, fibrotic
osteosclerosis - obliteration of BM space extramedullary
hematopoiesis - spleen later liver - PB leukoerythroblasticerytroid and granulocytic
precursors - 20 - progression to AML
32
Primary myelofibrosis (peripheral blood smear).
Two nucleated erythroid precursors and several
teardrop-shaped red cells (dacryocytes). Immature
myeloid cells present in other fields. An
identical picture - in other diseases producing
marrow distortion and fibrosis.
33
Leukaemia
- Acute myeloid lymphoblastic - B, T
- Chronic myeloid, lymphocytic B, T
34
Acute leukaemia (AL)
- Common acute course
- untreated death in weeks, months
- Problems symptoms result from
- A. failure of normal hematopoiesis anemia,
neutropenia, thrombocytopenia - B. infiltration of organs by neoplastic cells
- 1. Myeloid (adults)
- 2. Lymphoblastic (young B or T)
- further subdivision
- genetics, morphology, immunophenotype
35
Acute leukaemia
36
Acute myeloid leukaemia
- Categories
- AML with recurrent gen. abnormalities balanced
translocations, often complete remission,
favourable prognosis (fusion gene - chimeric
protein) - t(1517) AML M3 promyelocytic treatment
with transretinoic acid - t(8 21) or inversion of chromosome 16
- AML therapy related
- AML with multilineage dysplasia
- AML NOS- minim.differentiated
- Without maturation
- With maturation
37
Acute myeloid leukaemia
- FAB classification French American British
- M0 without maturation myeloblastic
- M1 without maturation
- M2 with maturation
- M3 promyelocytic now categorised rather
according to the genetics t(15 17) - M4 myelomonocytic
- M5 a monoblastic, b- monocytic
- M6 erythroid
- M7 megakaryoblastic
38
Myeloid sarcoma
- Tumour mass of immature myeloid cells
- Extramedullary (bone)
- Association - before or concurrently
- 1. AML (or as a relapse)
- 2. Chronic myelogenous leukaemia
- other myeloproliferative disorders
- 3. MDS
Extramedullary myeloid tumour, granulocytic
sarcoma, chloroma
39
Myeloid sarcoma
- Localization
- 1. Bones subperiosteal
- (skull, paranasal sinuses, sternum, ribs,
vertebrae, pelvis) - 2. Lymph nodes
- Skin
- Histological types
- A. Granulocytic
- B. Monoblastic
- C. Trilineage haematopoiesis
40
Myeloid sarcoma - poorly differentiated
- a high index of suspicion...
- Stains CHAE, MPO, lysozyme CD15, CD68,
CD117, CD43 (CD43 only!) - Differential diagnosis
- 1. Lymphoblastoma
- 2. Burkitt lymphoma
- 3. Large cell lymphoma
- 4. Small round cell tumours
- (neurobl., Ewing/PNET,
- medullobl.)
Lymphoblastoma
41
Myeloid sarcoma
- Prognosis
- If MPD, MDS as a blast transformation
- If AML as this AML
- If isolated curative radiotherapy
- prolonged survival
42
Precursor (lymphoblastic)B-cell neoplasmsB-acute
lymphoblastic leukaemia/lymphoblastic lymphoma
- 1. Leukaemia (more common) involves the bone
marrow and PB - 2. occasionally solid primary nodal or extranodal
mass /B-lymphopblastic lymphoma/ without PB and
BM involevement - - leukaemization possible. biologic unity of
B-ALL and B-LBL, division arbitrary
43
Precursor (lymphoblastic)B-cell neoplasms
- Small to medium sized cells
- scant cytoplasm, dispersed chromatin, and
inconspicuous nucleoli
44
Acute lymphoblastic leukemia/lymphoma.
Lymphoblasts condensed nuclear chromatin, small
nucleoli, and scant agranular cytoplasm
45
Lymphoblastic leukaemia
- More common B
- B-ALL children, but also adults relatively
frequent, good prognosis - Children 95 complete remission, 80 cured
/adults worse/ - Lymphoblastoma (LBL)
- More common T
- B-LBL rare
- T-LBL- rapidly growing mass in mediastinum,
adolescent male
46
Acute B-cell lymphoblastic leukaemia
- B-ALL children, but also adults relatively
frequent - B-LBL - much less common - skin, bone, soft
tissues, LN - Symptoms BM failure
- Enlarged LN, liver, spleen
- Antigenic profileTdT, CD10 (CALLA) various
degree of differentiation, B-antigens (CD79a,
CD20) - Genetic abnormalities prognostically important
- Good hyperdiploidy t (12, 21)
- Poor t(9, 22), hypodiploidy
- In general a good prognosis leukaemia
- Children 95 complete remission, 80 cured
/adults worse/