Management of Secondary Spontaneous Pneumothorax - PowerPoint PPT Presentation
1 / 1
Title:
Management of Secondary Spontaneous Pneumothorax
Description:
Cystic changes are prominent throughout the lungs with relative ... cancer, Pneumocystis jerovici, cystic fibrosis, tuberculosis or other lung diseases. ... – PowerPoint PPT presentation
Number of Views:300
Avg rating:3.0/5.0
Title: Management of Secondary Spontaneous Pneumothorax
1
Management of Secondary Spontaneous Pneumothorax
Randal L. Croshaw, MD, Scott Matherly, MD, James
M. Nottingham, MD, FACS
University of South Carolina Department of Surgery
The case for early definitive treatment The
recurrence rates of primary and secondary
pneumothoraces for patients in patients not
undergoing definitive management are 31.8 and
43, respectively. Patients that develop a
pneumothorax secondary to pulmonary Langerhans
cell histiocytosis have a 58 chance of
recurrence if not treated definitively. The
recurrence rates of pneumothorax due to AIDS or
CF are 11-65 and 50-79, respectively.
Mortality for secondary spontaneous pneumothorax
is 1.8 to 3.3 while mortality for primary
spontaneous pneumothorax is 0.06 to 0.09.
Spontaneous pneumothorax
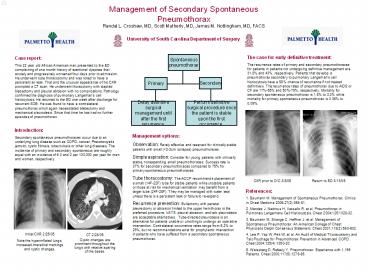
Case report This 22 year old African American
man presented to the ED complaining of one month
history of exertional dyspnea that acutely and
progressively worsened four days prior to
admission. He underwent tube thoracostomy and was
noted to have a persistent air leak. That and the
unusual appearance of his CXR prompted a CT scan.
He underwent thoracotomy with stapled blebectomy
and pleural abrasion with no complications.
Pathology confirmed the diagnosis of pulmonary
Langerhans cell histiocytosis. He returned to
the ED one week after discharge for recurrent
SOB. He was found to have a contralateral
pneumothorax which again necessitated blebectomy
and mechanical pleurodesis. Since that time he
has had no further episodes of pneumothorax.
Primary
Secondary
Delay definitive surgical management until after
the first recurrence.
Perform definitive surgical procedure once the
patient is stable upon the first occurrence.
Introduction Secondary spontaneous
pneumothoraces occur due to an underlying lung
disease such as COPD, cancer, Pneumocystis
jerovici, cystic fibrosis, tuberculosis or other
lung diseases. The incidence of primary and
secondary spontaneous are roughly equal with an
incidence of 6.3 and 2 per 100,000 per year for
men and women, respectively.
Management options Observation Rarely effective
and reserved for clinically stable patients with
small (lt2-3cm collapse) pneumothoraces. Simple
aspiration Consider for young patients with
clinically stable, nonexpanding small
pneumothoraces. Success rate is 37 for secondary
pneumothoraces compared to 75 for primary
spontaneous pneumothoraces. Tube thoracostomy
The ACCP recommends placement of a small
(14F-22F) tube for stable patients while unstable
patients or those at risk for mechanical
ventilation may benefit from a larger tube
(24F-28F). They may be managed with water seal
unless there is a persistent leak or failure to
re-expand. Recurrence prevention Bullectomy with
parietal pleurectomy or abrasion limited to the
upper hemithorax is the preferred procedure.
VATS, pleural abrasion, and talc pleurodesis are
acceptable alternatives. Tube-directed
pleurodesis is an alternative for patients unable
or unwilling to undergo an operative
intervention. Contralateral occurrence rates
range from 5.2 to 29, but no recommendations
exist for prophylactic intervention in patients
who have suffered from a secondary spontaneous
pneumothorax.
CXR prior to D/C 3/8/05
Return to ED 3/13/05
References 1. Baumann M. Management of
Spontaneous Pneumothorax. Clinics in Chest
Medicine 200627(2)369-81. 2. Mendez J, Nadrous
H, Vassallo R, et al. Pneumothorax in Pulmonary
Langerhans Cell Histiocytosis. Chest
20041251028-32. 3. Baumann M, Strange C,
Heffner J, et al. Management of Spontaneous
Pneumothorax An American College of Chest
Physicians Delphi Consensus Statement. Chest
2001119(2)590-602. 4. Lee P, Yap W, Pek W, et
al. An Audit of Medical Thoracostomy and Talc
Poudrage for Pneumothorax Prevention in Advanced
COPD. Chest 2004125(4)1350-20. 5. Weissberg D,
Refaely Y. Pneumothorax Experience with 1,199
Patients. Chest 2000117(5)1279-85.
- CT 2/28/05
- Cystic changes are prominent throughout the lungs
with relative sparing of the bases.
Initial CXR 2/25/05 Note the hyperinflated lungs,
increased interstitial markings and cystic
changes.