Reducing Decubitus Ulcers and Eliminating Restraints - PowerPoint PPT Presentation
1 / 36
Title:
Reducing Decubitus Ulcers and Eliminating Restraints
Description:
Two sessions each day in Phoenix: June 2, 5, 6, Sessions begin at 7:30 a.m. and 1 p.m. ... 1130 N. 22nd Ave., Phoenix. Tucson Location. ADHS Long Term Care Licensing ... – PowerPoint PPT presentation
Number of Views:171
Avg rating:3.0/5.0
Title: Reducing Decubitus Ulcers and Eliminating Restraints
1
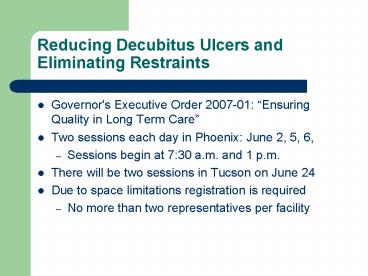
Reducing Decubitus Ulcers and Eliminating
Restraints
- Governor's Executive Order 2007-01 Ensuring
Quality in Long Term Care - Two sessions each day in Phoenix June 2, 5, 6,
- Sessions begin at 730 a.m. and 1 p.m.
- There will be two sessions in Tucson on June 24
- Due to space limitations registration is required
- No more than two representatives per facility
2
Reducing Decubitus Ulcers and Eliminating
Restraints
- Phoenix Location
- ADOT Human Resource Development Center
- 1130 N. 22nd Ave., Phoenix
- Tucson Location
- ADHS Long Term Care Licensing
- 400 W. Congress, 158, Tucson
3
Pressure Ulcers
4
Pressure Ulcer
- Is an area of skin that breaks down, usually over
a bony prominence (area where bones are close to
the skin), when a person is in one position for
too long without shifting their weight to
relieve pressure.
5
Pressure Ulcer
- Starts as an area of reddened skin, and without
relief of pressure will progress to an open sore,
and then a crater.
6
The Effects of Pressure
- Constant pressure against the skin reduces the
blood supply to that area, which supplies the
skin/tissue with nutrients and oxygen. Without
the nutrients and oxygen the tissue dies and a
pressure ulcer forms.
7
Other Causes
- Shear
- Occurs when skin moves in one direction, and the
underlying bone moves in another. This type of
movement stretches and tears cell walls and small
blood vessels.
8
Other Causes
- Friction
- Occurs when force is able to overcome the bodys
resistance to movement, even slight rubbing or
friction on the skin may cause minor pressure
ulcers.
9
Other Causes
- Moisture
- Caused by excessive perspiration or incontinence
can irritate or soften the skin and contribute to
the development of pressure ulcers
10
Staging
- Pressure sores are categorized by severity, from
Stage I (first sign) to Stage IV (worst)
11
Stage I
- Intact skin with non-blanchable (does not turn
white when pressed) areas of redness usually over
a bony prominence. Individuals with dark
pigmented skin may not have visible blanching,
the area may appear discolored.
12
Stage I
13
Stage I
14
Stage II
- Partial thickness loss, epidermis or topmost
layer of the skin is broken, presenting as an
abrasion or shallow open ulcer with a pink/red
wound bed, without necrotic (dead) tissue. The
ulcer may also present as an intact or open
blister.
15
Stage II
16
Stage III
- Full thickness tissue loss, damage to the tissue
extends through the dermis (second skin layer)
into the subcutaneous and fat tissue. Slough
(necrotic yellow or gray tissue that is
separating from living tissue) may be present.
17
Stage III
18
Stage IV
- Full thickness tissue loss, damage to the tissue
extends into the muscle and can extend as far
down as the bone. Slough or eschar (thick black
or dark brown leather like necrotic tissue) may
be present on some parts of the wound bed.
19
Stage IV
20
Unstageable
- Full thickness tissue loss in which the base of
the ulcer is covered by slough and/or eschar.
21
Unstagable
22
Unstagable
23
Where
- Pressure ulcers most commonly develop over bony
prominences like - elbow, heels, hips, ankles, sides of the knee,
shoulders blades, back, and the back of the head.
24
Pressure Areas
25
Pressure Areas
26
Pressure Areas
27
Identifying Who is at Risk
- Residents who are
- bedridden
- in a wheelchair most or all time
- unable to move certain parts of their body
without assistance - incontinent of bowel and/or bladder
- malnourished
- obese
28
Identifying Who is at Risk
- Residents who have
- dementia, Alzheimer's disease or other mental
disabilities - Diabetes
- a history of pressure ulcers
- vascular disease (poor blood flow)
- fragile skin
29
Preventive Measures
- Reposition residents at least every two hours to
relieve pressure. - Use items that can help reduce pressure --
pillows, sheepskin, foam padding - Provide healthy, well-balanced meals.
- Assist with daily range-of-motion exercises for
limited mobility residents - Limit moisture, residents who are incontinent
should be kept clean and dry.
30
Preventive Measures
- Residents who have any of the risk factors,
should be checked for pressure sores every day.
Look for reddened areas that when pressed, do not
turn white, blisters and sores.
31
Contact a Medical Professional
- When an area of skin
- turns red and does not blanch
- blisters
- forms an open sore
32
Contact a Medical Professional
- When
- A foul odor from the ulcer is first noticed
- Redness and tenderness around the ulcer is
noticed - Skin close to the ulcer is warm or swollen
- - Color or amount of drainage from the ulcer
changes
33
R9-10-722.C.1/723.D
- C. A licensee shall provide to each resident
receiving personal care services - 1. Skin maintenance to prevent and treat bruises,
injuries, pressure sores, and infections - This also applies to residents at the directed
level of care.
34
R9-10-722.A.4/723.B.3
- In order to accept or retain a resident who has a
stage 3 or stage 4 pressure sore, an Assisted
Living licensee must ensure - Written authorization for residency or continued
residency is signed and dated by the resident or
representative
35
R9-10-722.A.4/723.B.3 (Cont)
- The residents primary care provider examines the
resident, then signs and dates a statement
authorizing residency at the facility - This must be done every six months
36
R9-10-722.A.4/723.B.3 (Cont)
- The residents service plan is revised to include
the residents increased need for services - The resident is under the care of a nurse,
licensed home health agency or licensed hospice
agency - The facility is meeting the residents needs
- The facility documents the services provided
37
Questions