SelfDirected HIPAA Training Instructions - PowerPoint PPT Presentation
1 / 56
Title:
SelfDirected HIPAA Training Instructions
Description:
Colleague in the hospital and so you access the system to get a discharge date to send flowers ... How do you send health information (fax, e-mail, etc.) Make ... – PowerPoint PPT presentation
Number of Views:1290
Avg rating:3.0/5.0
Title: SelfDirected HIPAA Training Instructions
1
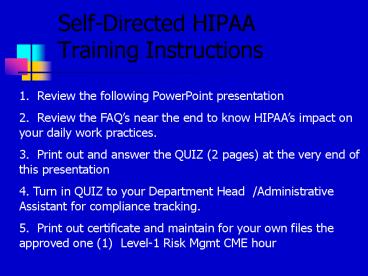
Self-Directed HIPAA Training Instructions
1. Review the following PowerPoint
presentation 2. Review the FAQs near the end to
know HIPAAs impact on your daily work
practices. 3. Print out and answer the QUIZ (2
pages) at the very end of this presentation 4.
Turn in QUIZ to your Department Head
/Administrative Assistant for compliance
tracking. 5. Print out certificate and maintain
for your own files the approved one (1) Level-1
Risk Mgmt CME hour
2
(No Transcript)
3
Content of Session
- What is HIPAA and why is it important?
- Examples of Breaches
- What rights do patients have under HIPAA?
- Safe Information Practices
- Privacy and Security Compliance
- How do you report a breach?
- Resources
4
What is HIPAA?
- Health Insurance Portability and Accountability
Act - Signed into Law August 21, 1996 (Public Law
104-191) - Significant impact on health care industry
- Goals To improve the efficiency and the
effectiveness of the health
care system - the establishment of standards and requirements
for the electronic transmission of certain health
information (eligibility, referrals, and
claims)and - create the first national legislation to give
every patient across the nation protection of
their health information
5
What Do You Have To Know?
- Stronger Massachusetts privacy laws are followed
over HIPAA rules in certain situations (like
those covering Mental Health, HIV, Aids, Alcohol
and Drug Abuse, Domestic Violence, Sexual
Assault, Genetic Testing) - Patients have the right to file a
complaint if they believe their
privacy rights have been
violated
6
What Do You Have To Know?
- What is confidential?
- Protected Health Information or PHI
- any information that identifies who you are
- (as little as name, address and social security
is PHI) - past, present or future physical or mental
health or
condition - type of treatment or services provided
- past, present, or future payment for care
provided
- Patients will have the right to file a grievance
or complaint if they believe their privacy rights
have been violated
7
Why is HIPAA important to Massachusetts General
Hospital?
- Maintaining patients trust in their caregivers
is critical to obtaining a complete history,
medical record, and carrying out an effective
treatment plan - It supports our mission
- Its the right thing to do
8
Protecting Patient Privacy
- As healthcare workers we see and
hear confidential information every
day on the job. - We get so accustomed to being around this kind of
information that its easy to forget how
important it is to keep it private - Privacy and confidentiality is a basic right in
our society. - Safeguarding that right is your ethical and legal
obligation
9
Failure to Protect Patient Privacy Can Have Dire
Consequences
- It has been documented that failure to protect
patient privacy has caused patients to - Lose Jobs
- Be Victims of False Rumors
- Lose Insurance Coverage
- Become Estranged from Friends and Family
- Lose Custody Battles
- Be harassed by the Media
- Some examples.
10
Examples of Breaches Big Breaches in the news
- An error in a University of Minnesota database
failed to suppress the names of deceased organ
donors on computer-generated letters to the 410
patients who received their kidneys (Report on
Patient Privacy, 3/02)
11
Examples of Breaches Small seemingly innocent
breaches, or activities that could lead to
breaches
- An employee checking the record of a friend or
family member, in order to see how they are doing - Leaving patient identifiable information on
computer when you bring the next patient into the
exam room - Neglecting to confirm accuracy of fax number
before sending identifiable health information - Colleague in the hospital and so you access the
system to get a discharge date to send flowers - A high profile patient comes in for tests and you
say to your colleague, guess who I just took care
of? Joe Celebrity
12
Examples of Breaches Small seemingly innocent
breaches, or activities that could lead to
breaches
- Leaving work at the end of the day and leaving
patient information out on your desk rather than
in a folder - Discussing patient information on your cell phone
in the Treadwell Library, cafeteria or on the
shuttle bus. - Not closing the exam room door or privacy curtain
when discussing patient information - Walking up to a computer and using it while
logged in under a co-workers password or not
logging off computer when you leave the area
13
Enforcement of HIPAA Office of Civil Rights
PRIVACY
Its the LAW!
- HIPAA calls for severe civil and criminal
penalties for noncompliance - fines up to 25K for multiple violations of the
same standard in a calendar year - fines up to 250K and/or imprisonment up to 10
years for deliberate misuses of individually
identifiable health information - Healthcare organizations must have sanctions in
place for their workforce and business associates
who violate their privacy policies
14
Patient RightsIn regard to their health
information
Receipt of Privacy Notice
- The right to receive a written notice of how
their health information
will be used and disclosed--this
is called the Privacy Notice - The Privacy notice must
- Contain patients rights and the covered
entities legal duties - Be made available to patients in print
- Be displayed at the site of service and posted on
our web site - Patients must receive a copy of our Privacy
Notice concerning the use/disclosure of their PHI
on the first date of service delivery, or as soon
as possible after an emergency
15
Patient RightsIn regard to their health
information
Receipt of Privacy Notice
- All new and established patients must receive a
MGH/Partners Privacy Notice one time only at
their initial visit following implementation. - We must ask patients to sign an Acknowledgement
form of having received the Privacy Notice or
document reasons why the
acknowledgement was not signed - The Acknowledgement form will be sent to Health
Information Services to be maintained in
patients medical record and recorded in the
electronic record
16
Patient RightsIn regard to their health
information
- The right to access their own record, and to
request that their record be amended if it
contains incorrect or incomplete information - The right to request a limitation on information
used and disclosed - such as their information blocked from the
hospital directories and unavailable for people
who call information to ask for them - or their religious preference blocked from clergy
- or to request that you limit what information you
may share with their family or friends
17
Patient RightsIn regard to their health
information
- The right to receive a list of disclosures
- we must track anyone we disclose information to
without a signed authorization from the patient - patients have the right to receive a list of
these disclosures - The right to sign an authorization
- prior to most non-routine uses or disclosures of
their health information - with employers for employment decisions,
- with life, disability, or other insurers,
- for marketing activities. and
- for targeted fundraising activities
18
Speaking of confidentiality agreements...
19
When is an Authorization to Release PHI Required?
- General Rule
- if the use or disclosure is for something other
than treatment, payment or hospital operations - Exceptions
- Specific authorization is required for use and
disclosure of specifically protected or
privileged information, such as HIV testing,
Genetic testing, Alcohol and Drug Abuse records
(Federal Confidentiality Rules 42 CFR Part2)
Domestic Violence Counseling, Sexual Assault
Counseling, Psychotherapy Notes - Disclosures required by law
20
Key Definitions under HIPAA You may use or
disclose PHI if it is for...
- Treatment providing, managing and coordinating
care consulting with other care providers and
referring a patient to other providers. - Payment providers request for reimbursement,
eligibility and medical necessity determinations,
claims management and related activities - Health Care Operations quality assessment and
improvement, evaluation of providers, training,
legal services, auditing, compliance, limited
marketing and fundraising activities and other
business and administrative operations.
21
Reasons for Releasing Confidential PHI
- Providers are required to report certain
communicable diseases to state health agencies. - The Food and Drug Administration (FDA) requires
that certain information about medical devices
that break or malfunction be reported. - To inform appropriate agencies during disaster
relief. - To inform family members or other identified
persons involved in the patient's care, or notify
them on patient location, condition or death
22
Reasons for Releasing Confidential PHI
- Providers are required to report suspected child
abuse - Police have the right to request certain
information about patients to determine whether
they are suspects in a criminal
investigation--MGH Police can verify need - The courts have the right to order providers to
release PHI - Providers must report cases of suspicious deaths
or certain suspected crime victims, such as
people with gunshot wounds.
23
Safe Information Practices
- Rule number one
- Any person to whom information is
communicated must - Be authorized to receive the information
- Have a legitimate need to know
- What can I do to protect need to know?
- Verify peoples identity and employee badge when
they come to the unit, pull a medical record or
ask for information - Remember that access to a system on the
computer does not imply that it is appropriate
to search any patient information that may be
stored within the system at will, simply to
satisfy curiosity
24
Safe Information Practices
- Confidential subjects are discussed
only in a private setting (not in
Treadway library, cafeteria, elevator, locker
rooms,etc.) - Cautious use of cellular phones, PDAs, e-mail
and faxes for confidential information - Hard copy documents are secured (kept out of
sight) of unauthorized persons
25
Safe Information Practices
- No dictating in the hallway outside the exam room
- Following MGH policies and procedures for release
and disclosure of health information - Write your medical note as if the patient were
reading it over your shoulder - Do not discuss care issues such as test results
with the exam room door open
26
Safe Information Practices
- Computer Security
- Never share passwords
- Click on the yellow lock at the
bottom right corner of your screen when
leaving a workstation - Make sure there is no prior patient information
left on the computer screen before you place the
next patient in the exam room
27
Safe Information Practices
- Computer Security
- Personal databases containing patient
information are prohibited unless - they contain de-identified information
(as per HIPAA definition), or - you have received an IRB waiver, or
other IRB approval - Diskettes with patient information are never
thrown out without being cleaned off
28
Safe Information Practices
Electronic Mail
- E-mail containing patient identifiable
information should not be transmitted over the
internet, as security cannot
be guaranteed, however - Follow best practice for confidentiality
- Explain this to patients before you agree to
communicate with them this way - Do not put patient name or identifier in subject
heading - Keep information to a minimum necessary
- Create a second auto-signature in your Outlook
e-mail with a confidentiality statement
29
Safe Information Practices
Electronic Mail
- E-mails using the intranet between
all Partners entities is secure - For example Outlook system we use daily
for e-mailing colleagues
at the Brigham or
Newton Wellesley Hospital is secure - Patient Gateway is secure
- E-mail guidelines on the MGH web site clinical
policy http//healthcare.partners.org/mgh/policies
/default.htm
30
Safe Information PracticesFaxing
- Faxes are the least controllable type of
communication - ALWAYS use a cover sheet with a confidentiality
statement and your location and phone number even
on internal faxes - Never leave faxes sitting on fax machines
unattended - It is critically important when faxing
information - to verify the sender has the correct fax number,
and - that the fax machine is in a secure location,
and/or the receiver is available immediately to
receive the fax
31
Somewhere outside the Partners Network
32
What can you do? Be on your guard
- Your responsibility for protecting
patient privacy and confidentiality does not
end with your work shift - Dont divulge any patient information when in an
informal atmosphere or social setting - If asked about a patient, simply reply Im
sorry, that information is confidential - Respect everyone as if they were your family
member!
33
How to Report a Privacy Concern or Breach
- Contact the Compliance Hotline to report a breach
anonymously (617) 726-1446 - or
- Health Information Services (617) 726-2465
34
Privacy Complaints/BreachesWhat you should tell
a Patient or Family Member
- A patient or family member can contact the
Office Manager (in the office practice) or the
MGH Patient Advocacy Office at (617) 726-3370
35
Privacy Resources To learn more.
- Intranet sites where privacy/HIPAA information is
available - HIPAA Central on Partners Web Site (all
employees) http//phsweb17.mgh.harvard.edu/opbud
get/hipaa/hipaa.asp
- Policies and Procedures/Forms
- FAQs/Training Resources
- MGH Policy Manuals
- Administrative Policy Manual
- Clinical Policy Manual
- Human Resource Manual
- Patient Gateway (patients)
- Policies and Procedures/Forms
36
Privacy Resources To learn more.
- Internet Sites
- Dept. of Health and Human Services
- http//aspe.hhs.gov/admnsimp/Index.htm
- http//www.hhs.gov/ocr/hipaa/whatsnew.html
- Mass Health Data Consortium
- http//mahealthdata.org
- Workgroup for Electronic Data Interchange (WEDI)
- http//www.wedi.org
37
Privacy Resources To learn more.
- MGH Contact Persons
- Deborah Adair, Director of HIS, Privacy Officer
- Maryanne Spicer, MGH Compliance Officer
- Eileen Bryan, HIPAA Manager, Privacy Office
- embryan_at_partners.org
- (617) 726-6360
38
QA Privacy
- What are examples of the minimum necessary rule
in your daily work do changes in practice need
to be made? - Patient Sign in sheets
- Appointment reminder calls
39
Answer -- YES and YES
- Sign in sheets are permitted, although they
should kept to minimum information, some examples - First name last initial or last three numbers of
Medical record number - Have a blank sheet covering list
- Place stickers over patients already taken care
of to remove name - use small single sheets that are then deposited
in a hanging folder on reception desk - Calls are permitted as long as patients are
notified through our MGH Privacy Notice and
patients agree to give primary phone contact - Remember minimum necessary information to get the
job done - Use professional judgement around
privileged/protected PHI
40
QA Privacy
- HIPAA allows identifiable health information to
be shared among Partners-owned (or controlled)
entities on a need-to-know basis for certain
purposes (without obtaining a signed
authorization). - What are these reasons?
- Example patient is brought by ambulance to the
Faulkner Hospital. The nurse in the ED calls and
asks for patients last discharge note.
41
Answer
- Identifiable health information may be shared
- among health care providers for TPO
- Treatment
- Payment
- Healthcare Operations
(QA/QI, Utilization Review,
Disease Management, Credentialing, Auditing,
Accreditation, etc.) - Since the information was needed by Faulkner
Hospital for treatment purposes this is allowed
without written authorization.
42
QA Privacy in Inpatient Floors
- Mary is transported by Medflight to MGH for
specialized care. She is admitted to White 7 and
being treated by a specialist. An employee from
Medflight calls the Nursing station on White 7
the following day and asks for follow up
information on Mary. - Can the nurse give Medflight the information they
are asking for?
43
Answer -- Absolutely YES!
- This is considered a business associate who
assists MGH in treatment and hospital operations.
- MedFlight needs the follow up information for
billing purposes and also to meet their own
requirement to report patient information to DPH. - Have a procedure in place for verifying identity
of the caller that is actually a
Medflight employee
44
QA Privacy in Job Roles
- Olivia is a Nurse in the O.R. She has completed
her evening shift and is changing in the locker
room. Another nurse coming on for the day says
she heard there was a bad accident and that the
patient was in surgery all night. She asks
Olivia what the blood alcohol level of the
patient was. - How should Olivia respond?
- What are the risks here?
45
Answer
- Olivia should ask herself if this meets the need
to know criteria, if the nurse coming on was not
going to be treating this patient then Olivia
should state that she cant discuss the case
because of confidentiality. - Employee should limit amount of PHI discussed in
open work areas such as the locker room,
cafeteria or nursing station.
46
Next Steps Recommendations
- Appoint a Compliance Privacy and Security
Official for your practice/department (Office
Manager) - Review current practices for how your department
uses or discloses protected health information - Do you get a valid written authorization when
required - How do patients amend their records
- Do you follow minimum necessary policy
- What guidelines do you have in place for
communicating health information over the
telephone - How do you send health information (fax, e-mail,
etc.)
47
Make a list of all Business Associates
If you outsource a certain service,
such as transcription, follow below guidance
- HIPAA Definition a person or organization that
performs or assists in the performance
of a function that involves the use or
disclosure of individually identifiable health
information - Review business associate contract for privacy
and security policies and procedures also what
sanctions will be taken if these policies are
breached - MGH Legal has drafted contract language for new
and amended business associate contracts-see
Partners Intranet Web site HIPAA Central to use
these templates and further guidance - Materials Management has created a log of all
hospital business associates and will be
reviewing and updating these contracts--compare
your list with Materials Management
48
Next Steps -- Recommendations Review high
risk areas identified in the survey
- location of computer monitors
- move to non public area
- order privacy filter from Staples
- Are charts/patient information in or near public
areas (door racks, reception desk, fax
or copy machine, etc) - Place so patient name is not visible if possible
- do not leave papers unattended and close and lock
doors as feasible - photocopying patient health information
- Play it safe and get written authorization from
patient - taking health information off-site
- only take information off site if absolutely
necessary - maintain the same level of privacy and security
standards off site -- dont leave out in viewable
location
49
Additional high risk areas
- discussions regarding patients scheduling
patient
procedures/tests near public area - limit details, keep voices down
- place white noise machines near public waiting
area - disposing of health information
- request more blue recycle bins for white paper
and gray recycle bins for colored paper from
environmental services - We shred all paper products put in these recycle
bins - Discussing patient information in open areas
- do not discuss in health club, library,
cafeteria, waiting room, locker room, shuttle
bus--be aware of your surroundings
50
Massachusetts General Hospital Privacy
and Confidentiality Guiding
Principles
HIPAA
- A practical interpretation of the HIPAA
regulation - A commonsense approach to this endeavor
- A positive change that does not impede quality
patient care and - Unquestionable concern for safeguarding our
patients
protected health information
51
Key Points Keep your actions reasonable
- Most importantly -- do not let HIPAA impede our
quality care and patients trust -- that is not
the goal of HIPAA - We already do a really good job at protecting
health information -- whats different -- we now
have a legal obligation - Patients will be more knowledgeable in regard to
accessing, copying, amending and tracking
disclosures of their own health information -- so
we must be knowledgeable too -- both as
employees and health consumers ourselves
52
Key Points Keep your actions reasonable
- All health information is protected whether it is
spoken, written in a record or written and stored
electronically - View every decision about use and disclosure of
health information through the lens of - Treatment
- Payment
- Hospital Operations and
- the Minimum Necessary information to get the job
done - If it meets this criteria HIPAA does not require
a change in our everyday work practices
53
Take pride and ownership in the fact that
Massachusetts General Hospital is concerned
about privacy and recognizes its importance in
providingquality healthcare. Above all honor
our patients trust Thank you !
- Eileen Bryan
- MGH HIPAA Privacy Manager
- Health Information Services
54
HIPAA QUIZ
1. HIPAAs privacy rule protects a patients
fundamental right to privacy and
confidentiality of a) Patient information in
electronic form b) Patient information in paper
form c) Patient information communicated
orally d) all of the above 2. Now that there is
a federal law protecting patient privacy, all
individual health information shares the same
level of protection, including psychotherapy
notes, HIV test results, genetic testing, sexual
assault, domestic violence,etc.) a) True b)
False
55
HIPAA QUIZ
3. Patients have the right to amend inaccurate
or incomplete information contained in their
individual health record a) True b) False 4.
Health information is considered confidential if
it identifies the patient and relates to a) A
persons past, present, or future physical or
mental health condition b) A persons
present health condition only c) A persons past
and present condition only
56
(No Transcript)