Day - PowerPoint PPT Presentation
1 / 91
Title: Day
1
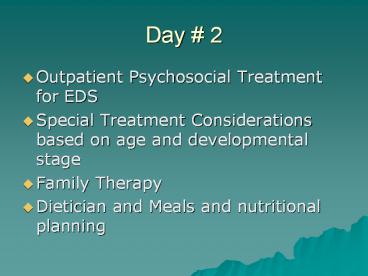
Day 2
- Outpatient Psychosocial Treatment for EDS
- Special Treatment Considerations based on age and
developmental stage - Family Therapy
- Dietician and Meals and nutritional planning
2
Working with Eating Disorder Patients in an
Outpatient Setting
- Elise Curry Psy.D.
- Program Manager
- UCSD IOP
3
Individual Therapy
4
Anorexia Nervosa Therapy Strategies
- Establish rapport
- Interpret function of symptoms needs
- Calculate weight goal (90 IBW)
- ½-1 lb per week weight gain in outpatient
- Encourage direct expression of feelings,
especially anger - Careful to allow patient true self expression
5
Anorexia Nervosa Therapy Strategies
- Address issues of expectations from others vs
individual wants - Explore fears with food and weight gain as having
some relationship to emotional experiences - Teach assertiveness skills. Helping patient say
no to things other than food. - Stimulate adolescent rebellion in other ways,
rather than starvation. (green hair, tattoos, R
rated movies, teenage clothing etc.) - Family, parent therapy esp with adolescents
6
Case study Janine
- Age 15
- Lives with mother
- Developed anorexia within past year
- Perfectionistic
- Make a mistake with a witness at the library
- Weight contract
- Weight restoration 12 lbs.
7
Therapy strategies for BN
- CBT, IPT, DBT
- Affect tolerance
- Engagement in other stress relieving and
pleasurable activities - Work on sitting with uncomfortable feelings,
rather than urge to get rid of feelings - Address issues of expectations from others vs
individual wants
8
Therapy strategies for BN
- Food/event diary
- Normalize eating, watching for deprivation
- Set goals for B/P episodes
- Trauma issues, shame
- Co morbid BLPD/O (BN)
9
Case example Shelly
- Age 25
- College Student
- C/S symptoms (name change)
- Purged through running
- Vow to herself at age 13
- Lacked age appropriate dating
- Assertiveness family phone conference
10
Group Therapy and Integrated Treatment
- Goal setting
- Structured on-site meals
- Meditation/Mindfulness
- Cognitive-behavioral therapy
- Process group
- Art therapy
- DBT
- Nutritional counseling
11
Goal setting
- Goal setting met, part, not met
- Mistake with a witness (perfectionism)
- Reducing the symptom B/P 1 max
- Letter to ED
- ED writes back
- Meal plan 3 meals plus 3 snacks helps to reduce
binge eating - Restrict - Binge - Purge (cycle)
- What can you do instead? Alternatives
- Binge if you want, but dont purge
- Challenge foods have a piece of cheesecake
- Foods are not good or bad incorporate desserts
into the meal plan
12
Process Group
13
(No Transcript)
14
Treatment considerations based on age
- Children (preteen)
- Adolescents
- Adults
- Chronic AN/BN
15
Important considerations
- Age of onset
- Time of low weight, linear history
- Developmental phase
- Involvement of others (family, spouse, children,
parents, etc)
16
What about the kids?
- Pre-pubertal Eating Disorder
- Childhood Onset Eating Disorder
- Early Onset Eating Disorder
17
What Are We NOT Talking About?
- DSM-IV Feeding and Eating Disorders of Infancy or
Early Childhood - Pica
- Rumination Disorder
- Feeding disorder of infancy or childhood
18
Anorexia NervosaDSM-IV
- Refusal to maintain body weight above a minimally
normal weight for age and height. - Intense fear of gaining weight or becoming fat
- Disturbance in the way ones body weight or shape
is experienced - Amenorrhea absence of at least three consecutive
menstrual cycles
19
Weight Loss vs Weight Maintenance
- DSM-IV criteria excludes children who have not
reached the critical level of - Malnutrition can lead to poor growth
20
Body Image
- May be more tricky to assess
- How can it be evaluated?
- Childrens expression of body image
- Standard tools
- Clinical Interview
- Somatic symptoms
- Abdominal pain or discomfort
- Feeling of fullness
- Nausea
- Loss of appetite
21
Amenorrhea
- Primary vs Secondary
- Pubertal delay
- Evaluation may include pelvic ultrasound
- Height
- Weight
- Weight/height ratio
- Ovarian volume
- Uterine volume
- Conventional target weight and weight/height may
be too low to ensure ovarian and uterine maturity
22
Alternative Criteria for ED in Children
Byant-Waugh and Lask 1995
- Alternative classification for the range of
eating disorders of childhood - Excessive preoccupation with weight or shape
and/or food intake which is accompanied by
grossly inadequate, irregular or chaotic food
intake
23
Byant-Waugh and Lask 1995 Criteria for Anorexia
Nervosa
- Failure to make appropriate weight gains, or
significant weight loss - Determined weight loss (e.g., food avoidance,
self-induced vomiting, excessive exercising,
abuse of laxatives). - Abnormal cognitions regarding weight and/or
shape. - Morbid preoccupation with weight and/or shape.
24
Related ED Behaviors in Children
- Anorexia nervosa
- Food avoidant emotional disorder
- Selective eating
- Functional dysphagia
- Bulimia nervosa
- Pervasive refusal syndrome
25
Early behavioral risk factors for EDs
- PICA BN
- Picky Eater BN, some AN
- Digestive problems AN
- Subsyndromal symptoms of EDs can predate
26
Incidence and Demographics
- Anorexia in this age range is considered to be
rare - Males may constitute a higher proportion of cases
in childhood as opposed to in adolescence or
adulthood - 19-30 of childhood cases
- 5-10 of adolescent or adult cases
27
WHY?
28
Biological
- Genetics
- Higher rate of AN, BN and ED NOS in first degree
relatives - Cross-transmitted
- High heritability
- Medication
- Trials suggest serotonin and dopamine systems
contribute
- Imaging
- Gordon et al, 1997
- 15 girls ages 8-16 with AN
- Regional cerebral blood blow radioisotope scans
- 13/15 had unilateral temporal lobe hypoperfusion
- Lask et al, 2005
- significant association between unilateral
reduction of blood flow in the temporal region
and - impaired visuospatial ability,
- impaired visual memory
- enhanced speed of information processing
29
Psychological
- Personality traits
- Anxious
- Obsessional
- Perfectionistic
- Susceptibility factors
- Obsessions
- Perfectionism
- Symmetry
- Exactness
- Negative affect, harm avoidance
- Preoccupations with weight, body image and food
30
SOCIAL
31
Prognosis
- Long term follow up of patients with early onset
anorexia nervosa (Bryant-Waugh et al, 1987) - 30 children with anorexia nervosa followed for
mean duration of 7.2 years - Mean age at onset 11.7 years
- 19/30 (60) with a good outcome
- 10/30 remained moderately to severely impaired
- Poor prognostic factors included
- Early age at onset (
- Depression during the illness
- Disturbed family life and one parent families
- Families in which one or both parents had been
married before
32
(No Transcript)
33
Family therapy
- Family Video and discussion
- Maudsley Family Therapy for Adolescents
- Systemic Family Therapy
34
Family Dynamics Video and Discussion
35
Maudsley Family Therapy
- Agnostic toward etiology
- Involves parents
- Food is medicine
- Initial focus on symptoms
- Parents are responsible for weight restoration.
- Non-authoritarian therapist stance
- Separation of child from illness
36
Maudsley Family Therapy
- Phase I (sessions 1 - 10) Weight restoration,
re-feeding focus. - Phase II (sessions 11 - 16) Transfer control
back to adolescent gradually. - Phase III (sessions 17 - 20) Focus on adolescent
developmental issues, termination.
37
Maudsley Family Therapy
- Session 1 Funeral session
- Goals engage the family, obtain history of how
AN came to be, find out how AN has affected each
family member, assess family functioning, reduce
blame, raise anxiety concerning AN. - Interventions Greet family in sincere but grave
manner, externalize the AN, orchestrate intense
scene, charge parents with the task of re-feeding.
38
Session 2 Family Meal
- Instructions to parents bring a meal that would
be appropriate for your childs nutritional
needs. - Goals assess family structure as it may affect
ability of parents to re-feed patient, provide an
opportunity for parents to successfully feed
patient, assess family process during meal. - Interventions bring the symptom alive and
present in the room, one more bite, align patient
with siblings for support.
39
Case Example BFT
- Madaline age 14
- Family members mom, dad, sister, patient
- Patients weight history
- Taking control back from patient.
- Patient reaction to loss of control.
- Rewards and consequences
- Patient weight progress over time.
40
Systemic Family Therapy
- Underlying belief if you fix the system, the
symptom will no longer be needed. - The eating disorder is serving a function in the
family. - The symptom bearer is trying to help the family
(unconsciously).
41
Methods for Systemic Family Therapy
- Circular questioning
- Therapist is curious observer, not expert.
- Discuss communication patterns within the family.
- Involve all family members in the discussion,
even small children. - Do not pathologize family or symptom bearer.
42
Case Example SFT
- Brianna age 16
- Family members mom, Gary, sister, patient
- Family of origin situation
- Current family living situation
- Symptoms of anorexia
- Function of the anorexia
- Changes in symptom over time
43
(No Transcript)
44
Meals/Dietitian
45
Handout nutritional assessment
46
(No Transcript)
47
(No Transcript)
48
(No Transcript)
49
Handout exercise plan
50
(No Transcript)
51
Weight Restoration Contract
- When to use
- Out patient level of care 0.5 1 lb per week
- Often includes exercise plan
- Parent/family/spouse informed
52
On site meals
- Exposure response prevention
- Challenge foods
- Peer support, peer pressure
- Rules at table
53
On site meals
- Structure of meal
- complete
- Behaviors to watch for
- Review of purpose for staff and patients
54
Dealing with meal challenges
- Food types to try
- Extinguishing behaviors
- Boost
- Limit setting on of boosts/ not eating meal on
site
55
Questions and Answers
56
(No Transcript)
57
(No Transcript)
58
Day 3
- Role Play training
- DBT/CBT
- Obesity/binge eating disorder
- Ends in Special Populations (pregnancy, athletes,
males)
59
DBT for Eating Disorders
60
Why DBT?
- Refine and change
- Behavioral
- Emotional
- Thinking patterns
- That cause suffering and distress.
61
Targets for Treatment
- 1. Interpersonal Chaos interpersonal
effectiveness training - 2. Labile affect emotional regulation training
- 3. Impulsiveness Distress tolerance training
- 4. Confusion about self and cognitive
dysregulation Mindfulness training
62
Interpersonal Chaos
- Examples
- 1. Intense, unstable relationships
- 2. Trouble maintaining relationships
- 3 panic,dread, anxiety over end of relationships
- 4. Frantic attempts to avoid abandonment.
63
Interpersonal Chaos
- Treatment goals
- 1. Learn to deal with conflicts
- 2. Learn to say no to unwanted requests/demands
- 3. Maintain self-respect and others respect.
64
Labile affect emotional regulation training
- Examples
- 1. Extreme emotional sensitivity
- 2. Ups and downs
- 3. Moodiness, intense emotional reactions
- 4. Chronic depression
- 5. Problems with anger (over and under-controlled)
65
Labile affect Treatment goals
- 1. Enhance emotional control
- 2. Remind members that to some extent we are who
we are, but we can learn to modulate emotions to
become a bit more relaxed.
66
Impulsivity Distress Tolerance Training
- Examples
- 1. Problems with drugs, alcohol, food, shopping,
sex, fast driving etc. - Treatment goals
- 1. Learn to tolerate distress
- 2. Explain connection btw distress and impulsive
behavior (often functions to reduce intolerable
distress)
67
Confusion about self and cognitive dysregulation
mindfulness training
- Examples
- 1.problems experiencing or identifying a self
- 2. Pervasive feelings of emptiness
- 3. Problems maintaining her/his own
opinions/feelings when around others - 4. Cognitive disturbances depersonalization,
dissociation - Treatment goals
- 1. Go within to find oneself
- 2. Learn to observe oneself
68
Structure of Group Sessions
- A. 50 homework, 50 new material, opening
mindfulness exercise and wind down. - B. Review diary cards
- C. Each person makes a practice commitment each
week - pick a skill to work on and use across a
variety of situations or for a recurrent
situation.
69
CBT for Eating Disorders
70
Distorted Beliefs
- There are good foods and bad foods.
- If I am fat, no one will love me.
- If I eat too much, I need to get rid of it by
purging. - If I eat this piece of cheesecake, I will be able
to see it on my body tomorrow. - You can never be too rich or too thin.
- Thinness equals happiness.
- Using laxatives gets rid of all the food.
- Purging gets rid of all the food.
- My worth is my weight.
- It is more important to be thin than anything
else. - Everyone hates fat people.
- Men like women who are skinny.
71
The Thin Commandments
- Carolyn Costin MFT
72
Recovery Beliefs
- My worth is not my weight.
- My body is an instrument, not an ornament.
- When I treat my body well, by eating 3 balanced
meals per day and exercising moderately, my body
will find its own set-point weight. - People come in all kinds of shapes and sizes. I
dont have to try to mold my body into a standard
set by the media or fashion industry. - I need some fat in my diet in order to have soft
skin, shiny hair, and be able to become pregnant
some day. - I can enjoy having a more curvy body, instead of
striving for thinness. - I am unique and special due to my inner
qualities. - Perfectionism only leads to disappointment, not
happiness.
73
(No Transcript)
74
Eating Disorders in special populations
- Pregnancy
- Males
- Obesity and Binge Eating disorder
75
ED and Pregnancy
- Reduced fertility, even after full recovery
- 20 pts at fertility clinics have EDs
- More likely to lie about ED behaviors during
pregnancy - High relapse rates after delivery
- Higher risk for PPD
76
Eating Disorders in Pregnancy
- Increase difficulty with weight gain
(psychological and physically) - Overall, most studies reveal improvement in
behaviors in pregnancy (for the greater good),
though often not enough - Risks low birth weight (and associated
features), prematurity, C-sections
77
Males and EDs
- Less common than in females, but increasing
(approx 10 of EDS occur in men) - They have a job or profession that demands
thinness. Male models, actors. - Cultural pressures to be V shaped
78
Males and EDS
- More in common with female EDs than differences
- Lower testosterone may predispose to ED
- Fears regarding sexuality
- More common in homosexual men
- Conflict over sexual identity
- Avoidant, passive, negative reactions from peers
as children
79
Males and EDs
- Athletes/profession with weight requirements
- 110 male to female ratio
- BED similar rates male/female, though women more
distressed about it, more guilt
80
Males and EDs
- They were fat or overweight as children
(different than females). - They have been dieting. Dieting is one of the
most powerful eating disorder triggers for both
males and females.
81
Males and EDs
- They participate in a sport that demands
thinness. Runners and jockeys are at higher risk
than football players and weight lifters. - Wrestlers who try to shed pounds quickly before a
match so they can compete in a lower weight. - Body builders are at risk if they deplete body
fat and fluid reserves to achieve high definition
82
Binge Eating Disorder
- Recurrent episodes of binge eating (see BN)
- The binge eating episodes are associated with
three (or more) of the following - Eating much more rapidly than normal
- Eating until feeling uncomfortably full
- Eating large amounts of food when not feeling
physically hungry - Eating alone because of being embarrassed by how
much one is eating - Feeling disgusted with oneself, depressed, or
very guilty after overeating - Marked distress regarding binge eating is present
- 2 days/week for 6 months
83
Obesity
- BMI 30
- 32.2 of American adults, increasing in children
- Increasing in past 30 years by 50 per decade
- Major successful treatment advances in treatment
of complications of obesity, but minimal success
in treatments for obesity itself
84
Is Obesity a psychiatric disorder (BED)?
- Medical/Metabolic issues
- Am J Psych 2007 Issues for DSM V Should
obesity be included as a brain Disorder - Major limitation to treatment of obesity is long
term behavioral compliance - Diets major cause of ED, including BED
85
BED and Neurochemistry
- Serotonin, endogenous opiates, cannabinoids
- Certain foods impact nucleus accombens DA,
opiate - Neuropsych IGT similar to addicts ie follow
immed reward over long term results during
gambling type tasks 9with excitable reward) - Individual biological risks genetic/heritability
86
Literature Review Treatment for BED
- International J of EDs May 2007
- 26 studies reviewed Med plus behav, meds alone,
behav alone - Meds plus BWL best, short term
87
Psychosocial treatments
- CBT
- CBT plus BWL
- BWL alone
- Group therapy
- Indiv therapy
- 12 step/self help
88
Medical treatments for BED/obesity
- Sibutramine
- Orlastat
- ? SSRIs, SNRis, TCAs
- ? Topiramate
- ? Zonisamide
- Acomplia
- Gastric Bipass
89
Special Assessment and Treatment Strategies for
Chronic AN
- Problems accumulate, may become irreversible
after as early as 6 mos - Poor Prognosis
- Risk benefit assessment of ED
- Harm reduction
90
Treatment issues in Chronic EDs
- Legal aspects
- Case examples
91
Final Question and Answer Session